Feasibility of Non-contact Noise Cancellation for Medical Device Alarms in Intensive Care Unit: An In Vitro Experiment
Nao Sonoda1*, Kiyotaka Fujii2, Akiko Morimoto1
1Graduate School of Nursing, Osaka Metropolitan University, Osaka, Japan
2School of Allied Health Sciences, Kitasato University, Kanagawa, Japan
*Correspondence to: Nao Sonoda, PhD, RN, Graduate School of Nursing, Osaka Metropolitan University, 3-7-30 Habikino, Habikino-city, Osaka, 583-8555, Japan; Email: sonoda@omu.ac.jp
Abstract
Objective: Medical device alarms in intensive care units (ICUs) are essential but their constant noise contributes to sleep disturbance and delirium in patients, jeopardizing their health and recovery. Therefore, improving the sound environment for patients in the ICU is crucial. This fundamental experiment investigated the potential of non-contact noise cancellation to reduce the noise level from medical device alarms in patients’ ears. We tested whether non-contact noise cancellation using a loudspeaker reduced the noise level of medical device alarms.
Results: The electrocardiogram sound from the bedside monitor was highest around 1kHz, while, the alarm sound from the syringe pump peaked around 4kHz. Non-contact noise cancellation using the loudspeaker reduced the electrocardiogram sounds emitted from the bedside monitor by more than 15decibel (dB) and the alarm sounds from the syringe pump by more than 10dB.
Conclusion: A 10dB change doubles or halves the perceived loudness, making the over 10dB reduction achieved for medical device alarms in this study highly significant. The results of this experimental study demonstrate the promising potential of noise-cancelling loudspeakers for improving patient comfort and well-being in ICUs.
Keywords: Noise, sound environment, non-contact noise cancellation, medical device alarm, ICU
1 INTRODUCTION
Medical device alarms in intensive care units (ICUs) are essential. However, their constant noise contributes to sleep disturbance and delirium in patients, jeopardizing their health and recovery[1-6]. Patients with delirium are at an increased risk of dying during admission, longer stays in the hospital, and cognitive impairment after discharge[7]. Therefore, it is important to improve the sound environment for patients in the ICU.
The World Health Organization recommends that noise levels (LAeq) should not exceed 35 decibel (dB) during the day and 30-40dB at night in hospital environments[8]. However, LAeq in the ICU are frequently reported to be in the range of 45-70dB, with peaks exceeding 85dB[4-6,9-13]. Although the alarm volume can be reduced from the default setting in the ICU, where patients are usually in critical condition, low-volume alarms may miss vital alerts, making medical professionals such as nurses anxious[14]. Therefore, it is necessary to reduce LAeq perceived by patients without compromising medical professionals’ awareness.
Noise reduction strategies include passive noise cancellation (e.g., earplugs), which physically prevents outside sounds from entering the ear, and active noise cancellation, which reduces the noise level in a particular area by sending a negative-phase sound. Earplugs are the commonest measure; however, the majority of studies related to the use of earplugs have found no benefit on objective sleep outcomes[15]. Conversely, regarding active noise cancellation, an experimental study reported that commercially available noise-cancelling headphones reduced LAeq in an ICU environment by 6.8dB[16]. However, noise-cancelling headphones and earphones are not suitable for patients in the ICU with poor general condition, who are at risk of developing pressure ulcers, or for those with head trauma.
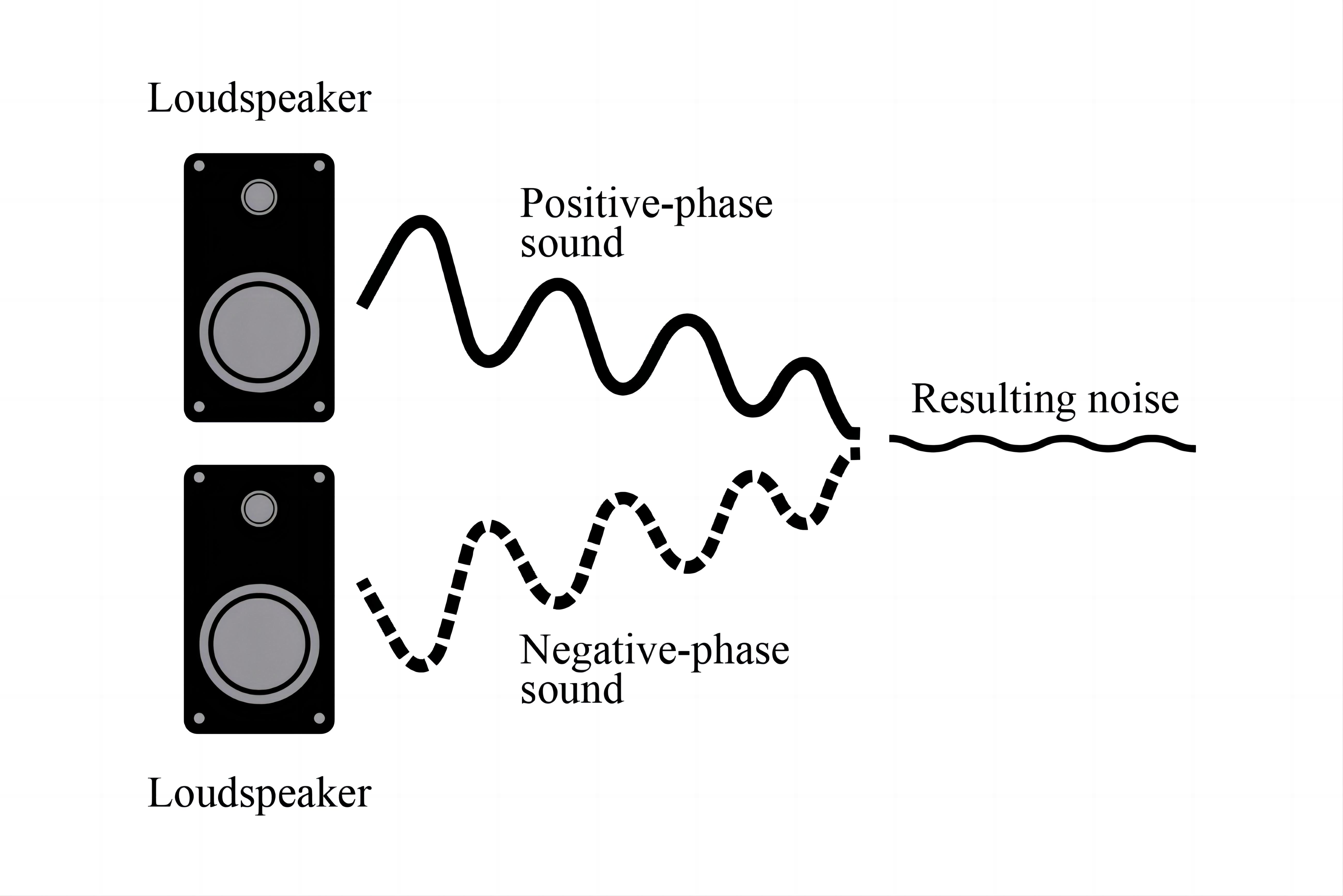
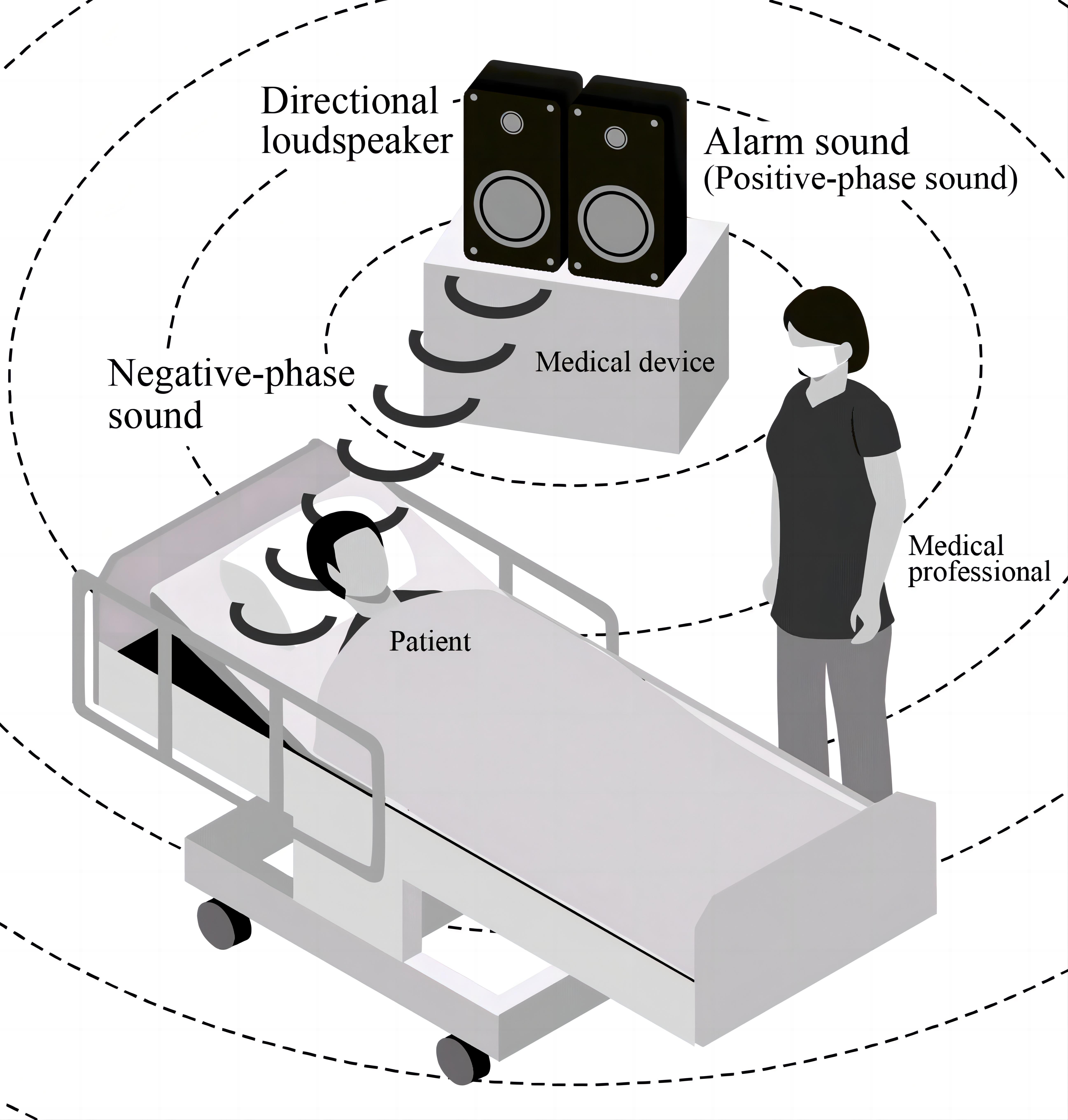
Sound is a pressure wave consisting of alternating periods of compression and rarefaction. The active noise cancellation concept relies on the superposition principle: a noise-cancelling loudspeaker emits a sound wave with the same amplitude but with an inverted phase (negative-phase sound) relative to the original sound (positive-phase sound). The waves combine to form a new wave in a process called interference and effectively cancel each other out (Figure 1). A loudspeaker may enable non-contact noise cancellation in patients in the ICU.
|
Figure 1. A noise reduction method using a noise-canceling loudspeaker.
As a fundamental experiment for developing non-contact noise cancellation to reduce the medical device alarm LAeq around patients’ ears, our study tested whether non-contact noise cancellation using a loudspeaker reduced the noise level of medical device alarms.
2 METHODS
We measured and analyzed medical device alarm sounds in Experiment 1 and created negative-phase sounds. In Experiment 2, we tested whether non-contact noise cancellation using a loudspeaker reduced the noise level of medical device alarms.
2.1 Experiment 1 (Characterization of Alarm Sounds)
2.1.1 Experiment Location
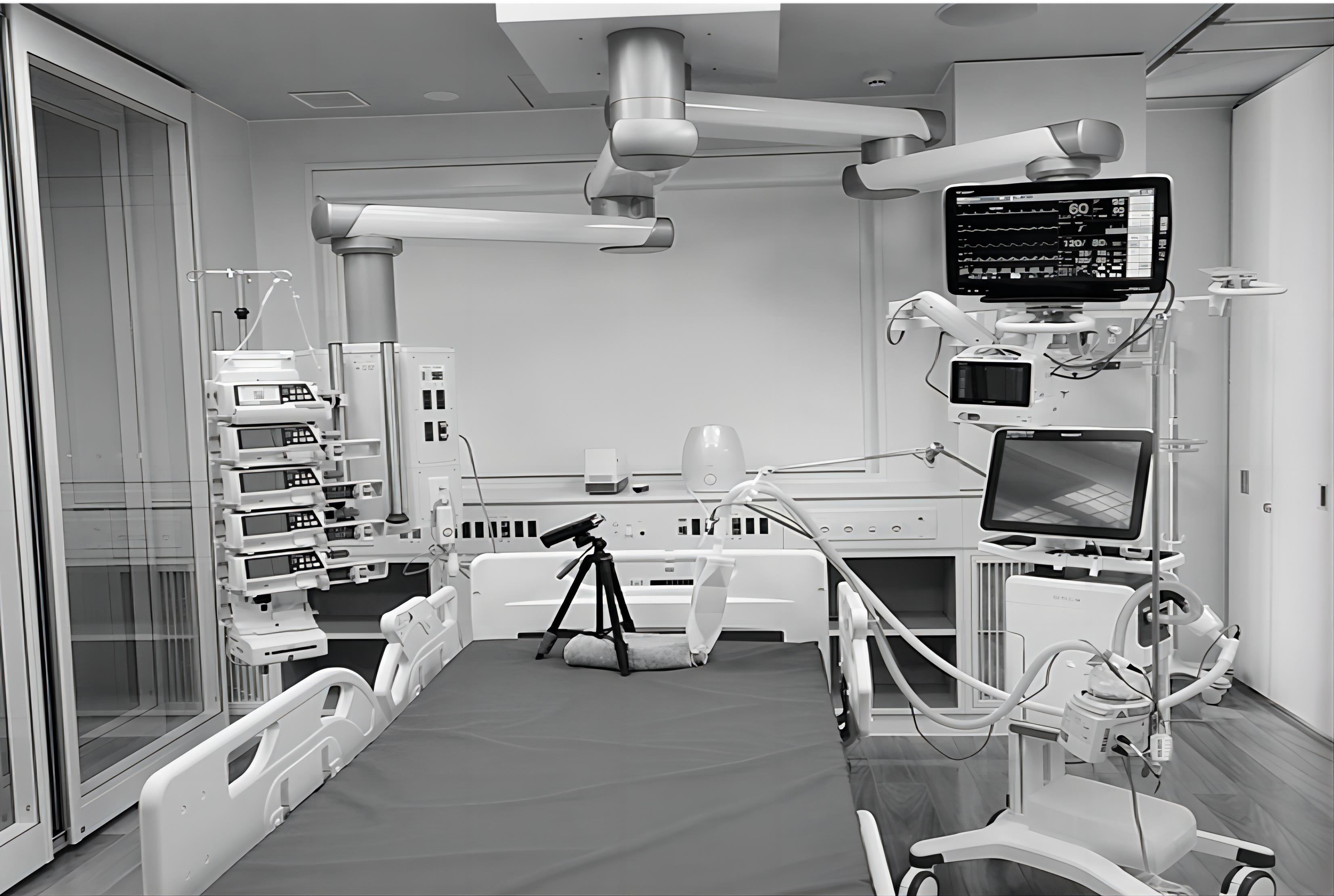
Experiment 1 was conducted in a simulated ICU environment (ICU Room at the Kobe International Living Medical Center, Hyogo, Japan) (Figure 2) in March 2020.
|
Figure 2. A simulated ICU environment.
2.1.2 Medical Device Alarms
We measured the electrocardiogram sounds (volume 2, default setting) from a bedside monitor and alarm sounds (volume 2, default setting) from a syringe pump, representing high-frequency and simple alarm sounds commonly used in ICUs.
2.1.3 Measurement and Analysis
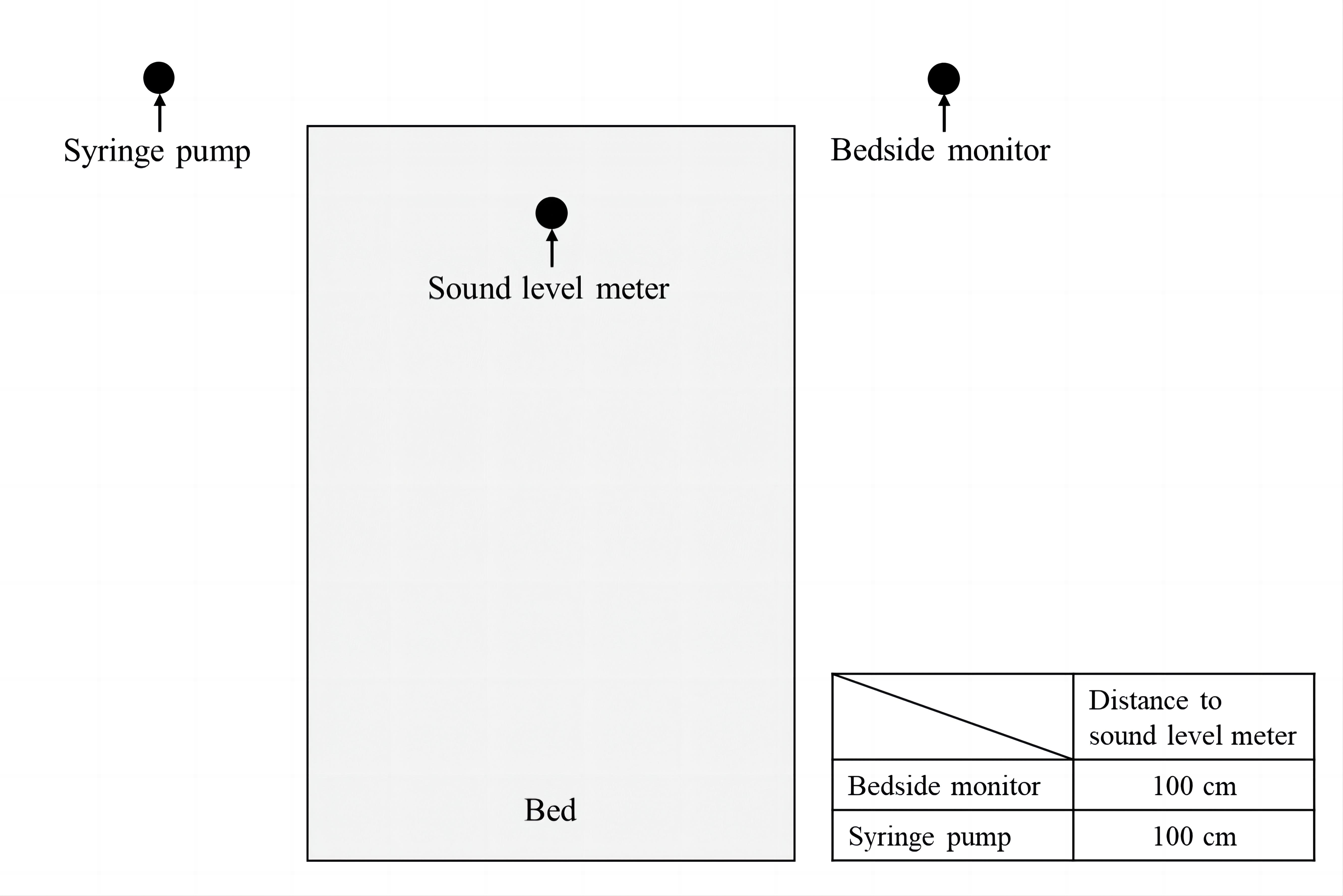
On the day of the measurement, no one was allowed on the floor except for the investigators. Additionally, all air conditioners and devices on the floor were turned off except for the medical devices to be measured. Measurements were recorded 100cm from the loudspeaker of each medical device (pillow position on the bed) (Figure 3). Further, each alarm sound was recorded for 10s using a sound level meter (NL-22, RION Corporation, Tokyo, Japan), and the LAeq (dB) and LAeq (dB) per frequency band were calculated. LAeq is the A-weighted equivalent continuous sound level (dB), and is a measure averaging noise exposure over a given period of time. Measurements were repeated thrice in the same environment.
|
Figure 3. Recording environment.
2.2 Experiment 2 (Non-contact Noise Cancellation Test)
2.2.1 Experiment Location
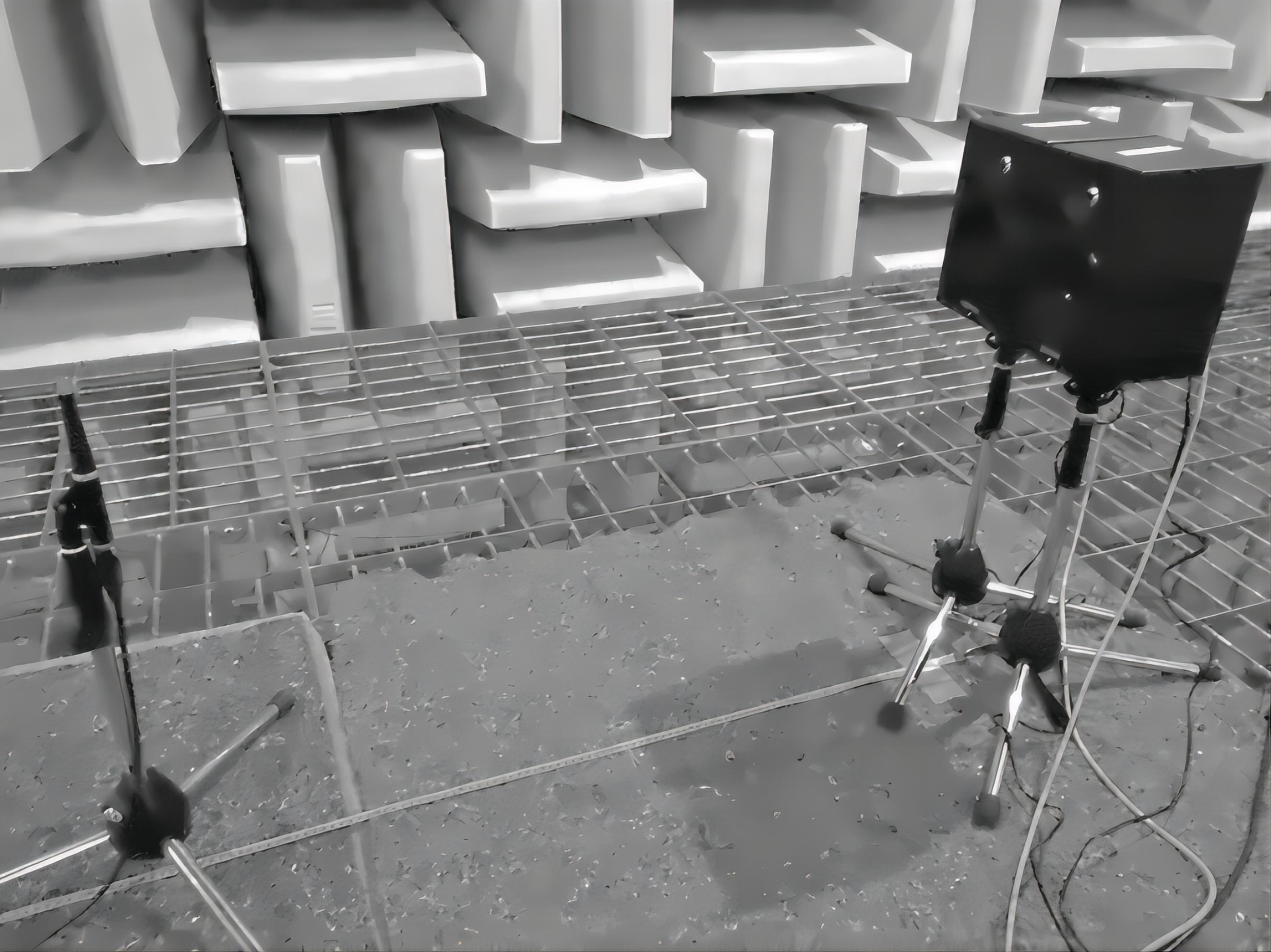
Experiment 2 was conducted in an anechoic chamber (Hyogo, Japan) in December 2020 to experimentally and accurately evaluate noise reduction.
2.2.2 Positive-phase and Negative-phase Sounds
We used the electrocardiogram sounds from the bedside monitor and alarm sounds from the syringe pump obtained in Experiment 1. Negative-phase sounds were created for each alarm sound obtained in Experiment 1 using Audacity (version 2.1.3) (Audacity, New Delhi, India).
2.2.3 Measurement and Analysis
We tested whether non-contact noise cancellation using a loudspeaker reduced the noise level of each alarm. The following devices and software were used in the experiment: two loudspeakers (MSP3, Yamaha Corporation, Hamamatsu, Japan), a sound playback software (Live 9.7.7, Ableton Corporation, Berlin, Germany), a measurement microphone (Type4007, Bruel & Kjaer Corporation, Nærum, Denmark), and a sound measurement software (Smaart 8.4.3.1, Rational-Acoustics Corporation, Woodstock, CT, USA). The two loudspeakers were placed in parallel (Figure 4), with the measurement microphone in front of them. While one loudspeaker played positive-phase sounds (alarm sounds obtained in Experiment 1), the other loudspeaker played negative-phase sounds.
|
Figure 4. Placement of two loudspeakers in the anechoic chamber.
First, the positive-phase sound pressure level was set to 60dB at the 50cm point, and the LAeq was measured every 10cm between 50cm and 100cm points when only the positive-phase sound was played for 10s. Furthermore, the LAeq was measured at the same points with both positive- and negative-phase sounds playing simultaneously for 10s. Finally, the difference (dB) between “the LAeq when only the positive-phase sound was played” and “the LAeq when both positive- and negative-phase sounds were played simultaneously” was calculated.
3 RESULTS
3.1 Characterization of Alarm Sounds (Experiment 1)
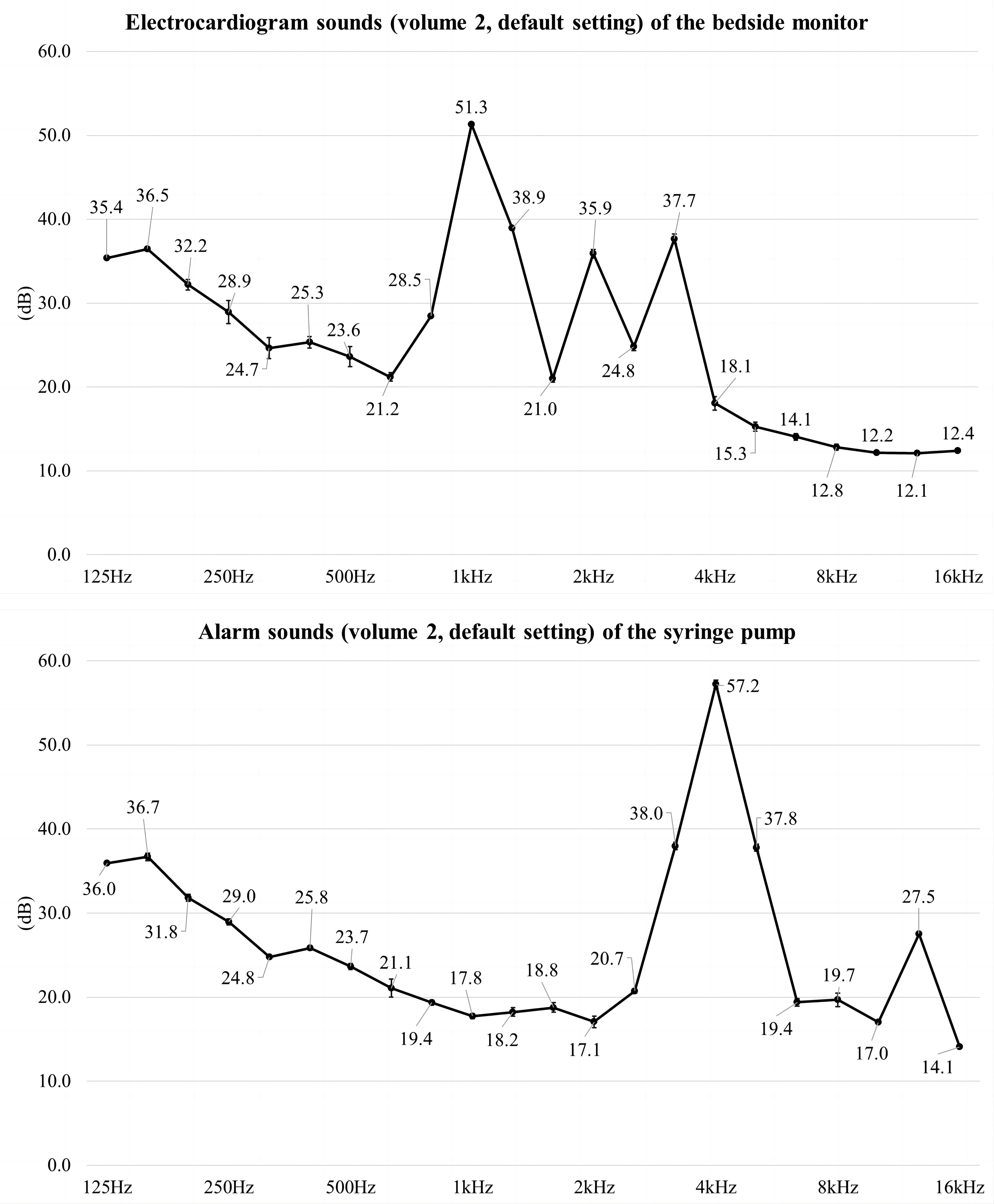
Mean LAeq of three measurements for both electrocardiogram sounds and alarm sounds at 100cm from their respective loudspeakers exceeded 50dB (Table 1). Mean LAeq of three measurements for each frequency band is shown in Figure 5. The electrocardiogram sound (volume 2, default setting) from the bedside monitor was high in dB around 1kHz. Meanwhile, the alarm sound (volume 2, default setting) from the syringe pump was high in dB around 4kHz.
Table 1. Electrocardiogram Sounds From the Bedside Monitor and Alarm Sounds From the Syringe Pump
|
Electrocardiogram Sounds (Volume 2, Default Setting) from the Dedside Monitor |
Alarm Sounds (Volume 2, Default Setting) from the Syringe Pump |
LAeq for 10s (dB) |
|
|
1st measurement |
52.2 |
58.0 |
2nd measurement |
52.1 |
58.9 |
3rd measurement |
51.9 |
58.1 |
Mean LAeq of three measurements (dB)* |
52.1±0.2 |
58.3±0.5 |
Notes:*Mean ± standard deviation.
|
Figure 5. Mean LAeq of three measurements of each frequency band.
LAeq is the A-weighted equivalent continuous sound level (dB), and is a measure averaging noise exposure over a given period of time.
Measurements were performed at a distance of 100cm from the loudspeaker of each medical device (pillow position on the bed).
3.2 Non-contact Noise Cancellation Test (Experiment 2)
The degree of reduction in the noise level of each alarm due to non-contact noise cancellation using a loudspeaker is shown in Table 2. The difference at the 100cm point was -16.2dB for the electrocardiogram sounds from the bedside monitor and -11.2dB for the alarm sounds from the syringe pump. Notably, both sounds experienced reductions exceeding 15dB and 10dB, respectively, at all points from 50cm to 100cm (average reductions: -17.3dB for electrocardiogram, -14.3dB for alarm).
Table 2. Degree of Reduction in the Noise Level of Each Alarm Due to Non-contact Noise Cancellation Using the Loudspeaker
|
50cm |
60cm |
70cm |
80cm |
90cm |
100cm |
Electrocardiogram sounds from the bedside monitor |
|
|
|
|
|
|
LAeq for 10s when only the positive-phase sound was played (dB) |
60.0 |
60.4 |
59.9 |
59.1 |
57.6 |
54.6 |
LAeq for 10s when positive- and negative-phase sounds were played simultaneously (dB) |
40.1 |
40.1 |
43.7 |
43.7 |
41.7 |
38.4 |
Difference (dB) |
-19.9 |
-20.3 |
-16.2 |
-15.4 |
-15.9 |
-16.2 |
Alarm sounds from the syringe pump |
|
|
|
|
|
|
LAeq for 10s when only the positive-phase sound was played (dB) |
60.0 |
57.1 |
56.9 |
55.9 |
55.4 |
54.3 |
LAeq for 10s when positive- and negative-phase sounds were played simultaneously (dB) |
42.5 |
41.5 |
37.3 |
45.6 |
43.7 |
43.1 |
Difference (dB) |
-17.5 |
-15.6 |
-19.6 |
-10.3 |
-11.7 |
-11.2 |
LAeq is the A-weighted equivalent continuous sound level (dB), and is a measure averaging noise exposure over a given period of time.
4 DISCUSSION
The electrocardiogram sounds (volume 2, default setting) emitted from the bedside monitor were characterized by a high dB level approximately 1kHz, exceeding 50dB at a distance of 100cm from the monitor’s loudspeaker. Notably, these sounds were reduced by more than 15dB owing to non-contact noise cancellation while using the loudspeaker. Similarly, the alarm sounds (volume 2, default setting) from the syringe pump, characterized by a high dB level approximately 4kHz and exceeding 50dB at a distance of 100cm from the loudspeaker of the syringe pump, were attenuated by over 10dB through non-contact noise cancellation.
Despite the increased emphasis on noise reduction in hospitals, hospital noise, particularly in ICUs, is a steadily worsening problem[17]. Previous studies have reported that the main noise sources in the ICU are medical device alarms and the voices of medical professionals[14,18-22]. Additionally, electronic sounds, such as alarms, have a greater negative effect on sleep disruption compared to human voices[23]. Moreover, frequent sound peaks (abrupt sound elevation exceeding 10dB) are the commonest cause of noise-induced arousal[24]. Notably, a 10dB change doubles or halves the perceived loudness, making the over 10dB reduction achieved for medical device alarms in this study highly significant. Our findings highlight the promising potential of noise-canceling loudspeakers to address this critical issue, and non-contact noise cancellation also has advantages in infection prevention.
The noise reduction recorded in this study surpassed the noise reduction (6.8dB reduction) achieved with commercially available noise-cancelling headphones in a previous experimental study[16]. We attribute this improvement to the likely creation of negative-phase sounds specifically for each alarm sound. Moreover, in this study, the electrocardiogram sounds of the bedside monitor showed more noise reduction than the alarm sounds from the syringe pump. The inherent characteristics of active noise cancellation, which performs better at lower frequencies. This may explain why the alarm sounds from the syringe pump, characterized by high dB levels (approximately 4kHz), are less likely to be reduced.
Conventional loudspeakers diffuse sound in all directions. However, in recent years, directional loudspeakers, which transmit sound in a straight line, have been utilized in everyday situations. In the future, the use of directional loudspeakers sending sound to a precise location may create a system that reduces the noise level perceived by the patient without inhibiting alerts to medical professionals (Figure 6).
|
Figure 6. Conceptualization of a future system that uses directional loudspeakers to reduce the noise level perceived by patients without inhibiting alerts to medical professionals.
4.1 Limitations
This study had some limitations. It was a fundamental experiment for developing non-contact noise cancellation to reduce the noise level around patients’ ears caused by medical device alarms. However, it is impossible to infer noise reduction in an actual ICU. Additionally, the alarm sounds tested in this study were limited.
5 CONCLUSION
In conclusion, this experimental study provides compelling evidence that non-contact noise cancellation using the loudspeaker reduced the electrocardiogram sounds emitted from the bedside monitor by more than 15dB and the alarm sounds from the syringe pump by more than 10dB. The results of this study demonstrate the promising potential of noise-cancelling loudspeakers for improving patient comfort and well-being in ICUs. Further in vitro experiments are needed for other medical device alarms such as ventilators. Additionally, Further experiments in the actual ICU are needed to develop non-contact noise cancellation.
Acknowledgements
We were grateful to all investigators in this experimental study. We thanked Yuionn Corporation and Japan Noise Survey Company for their technical support. This work was supported by the Fund from the Terumo Life Science Foundation.
Conflicts of Interest
The authors declared no conflict of interest.
Ethical Approval
This study did not involve human participants and did not require approval from the institutional review board.
Author Contribution
Sonoda N contributed to conceptualization, data collection, analysis, funding acquisition, project administration, and writing of the original draft. Fujii K contributed to conceptualization, data collection, analysis, funding acquisition, review, and editing. Morimoto A contributed to conceptualization, data collection, funding acquisition, project administration, review, and editing. All authors thoroughly reviewed and endorsed the final version of the manuscript.
Abbreviation List
dB, Decibel
ICU, Intensive care unit
LAeq, Noise levels
References
[1] Xie H, Kang J, Mills GH. Clinical review: The impact of noise on patients' sleep and the effectiveness of noise reduction strategies in intensive care units. Crit Care, 2009; 13: 208.[DOI]
[2] Figueroa-Ramos MI, Arroyo-Novoa CM, Lee KA et al. Sleep and delirium in ICU patients: a review of mechanisms and manifestations. Intensive Care Med, 2009; 35: 781-795.[DOI]
[3] Sangari A, Emhardt EA, Salas B et al. Delirium Variability is Influenced by the Sound Environment (DEVISE Study): how changes in the intensive care unit soundscape affect delirium incidence. J Med Syst, 2021; 45: 76.[DOI]
[4] Aydın Sayılan A, Kulakaç N, Sayılan S. The effects of noise levels on pain, anxiety, and sleep in patients. Nurs Crit Care, 2021; 26: 79-85.[DOI]
[5] Bani Younis M, Hayajneh F, Alshraideh JA. Effect of noise and light levels on sleep of intensive care unit patients. Nurs Crit Care, 2021; 26: 73-78.[DOI]
[6] Guisasola-Rabes M, Solà-Enriquez B, Vélez-Pereira AM et al. Noise levels and sleep in a surgical ICU. J Clin Med, 2022; 11: 2328.[DOI]
[7] Salluh JI, Wang H, Schneider EB et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ, 2015; 350: h2538.[DOI]
[8] Berglund B, Lindvall T, Schwela DH. Guidelines for community noise. Geneva: World Health Organization; 1999. Accessed 1 June 2024. Available at:[Web]
[9] Pisani MA, Friese RS, Gehlbach BK et al. Sleep in the intensive care unit. Am J Respir Crit Care Med, 2015; 191: 731-738.[DOI]
[10] Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care, 2013; 17: R187.[DOI]
[11] Cordova AC, Logishetty K, Fauerbach J et al. Noise levels in a burn intensive care unit. Burns, 2013; 39: 44-48.[DOI]
[12] Elliott RM, McKinley SM, Eager D. A pilot study of sound levels in an Australian adult general intensive care unit. Noise Health, 2010; 12: 26-36.[DOI]
[13] Morales-Cané I, Moral-Arroyo JA, Debbia F et al. Impact of sound levels on physiological and consciousness state of cardiovascular patients. Nurs Crit Care, 2022; 27: 240-250.[DOI]
[14] Pal J, Taywade M, Pal R et al. Noise pollution in intensive care unit: a hidden enemy affecting the physical and mental health of patients and caregivers. Noise Health, 2022; 24: 130-136.[DOI]
[15] Hu RF, Jiang XY, Chen J et al. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst Rev, 2015; 10: CD008808.[DOI]
[16] Gallacher S, Enki D, Stevens S et al. An experimental model to measure the ability of headphones with active noise control to reduce patient's exposure to noise in an intensive care unit. Intensive Care Med Exp, 2017; 5: 47.[DOI]
[17] Xyrichis A, Wynne J, Mackrill J et al. Noise pollution in hospitals. BMJ, 2018; 363: k4808.[DOI]
[18] Konkani A, Oakley B. Noise in hospital intensive care units: a critical review of a critical topic. J Crit Care, 2012; 27: e1-e9.[DOI]
[19] Tegnestedt C, Günther A, Reichard A et al. Levels and sources of sound in the intensive care unit - an observational study of three room types. Acta Anaesthesiol Scand, 2013; 57: 1041-1050.[DOI]
[20] Stafford A, Haverland A, Bridges E. Noise in the ICU. Am J Nurs, 2014; 114: 57-63.[DOI]
[21] Martinez FE, Poulter AL, Seneviratne C et al. ICU patients’ perception of sleep and modifiable versus non-modifiable factors that affect it: a prospective observational study. J Clin Med, 2022; 11: 3725.[DOI]
[22] Mori C, Boss K, Indermuhle P et al. Is it noise? Factors linked with sleep interruption in hospitalized patients. Clin Nurse Spec, 2021; 35: 199-207.[DOI]
[23] Buxton OM, Ellenbogen JM, Wang W et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med, 2012; 157: 170-179.[DOI]
[24] Gabor JY, Cooper AB, Crombach SA et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med, 2003; 167: 708-715.[DOI]
Copyright © 2024 The Author. This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.




 Copyright ©
Copyright ©