Parents' Knowledge regarding the Significance of Immunization for Children: A Systematic Review
Mohammad Yahya Ayoub1, Suhair Al-Ghabeesh2*![]()
1Department of Corporate Nursing Operations, Dr. Sulaiman Al-Habib Group Company, Riyadh, Saudi Arabia
2Faculty of Nursing, Al-Zaytoonah University of Jordan, Amman, Jordan
*Correspondence to: Suhair Al-Ghabeesh, PhD, Professor, Faculty of Nursing, Al-Zaytoonah University of Jordan, Airport Street, Amman, 11733, Jordan; Email: suhair_alghabeesh@yahoo.com
Abstract
Background: Parents often lack specific knowledge about vaccines schedules, lesser-known diseases, and vaccines safety. Enhancing parents’ knowledge about immunization is essential for informed decision-making and promoting vaccine acceptance.
Objective: This systematic review aimed to identify the parents’ knowledge about immunization, including their understanding of immunization concepts, knowledge gaps, and misconceptions. The review explored the factors influencing parents’ knowledge, such as socio-demographic factors, cultural and religious beliefs, sources of information, healthcare provider communication, and vaccine hesitancy.
Methods: A literature search was conducted by viewing relevant studies via computerized searching through PubMed, Scopus, and Embrace.
Results: The number of reviewed studies was 137, all in English and none in Arabic. Only 47 of them were selected based on inclusion criteria. Misconceptions, such as concerns about vaccine ingredients or false associations with adverse events, contribute to vaccine hesitancy. Socio-demographic factors influence parents’ knowledge, including age, education, and income. Cultural and religious beliefs shape their understanding, and sources of information, such as healthcare providers and media, play a significant role.
Conclusion: Addressing knowledge gaps and misconceptions requires strengthening healthcare provider communication, targeted educational interventions, regulation of online information, collaboration with community stakeholders, and longitudinal research.
Keywords: parents’ knowledge, immunization, vaccination
1 INTRODUCTION
Immunization, or vaccination, is a crucial public health intervention to prevent infectious diseases and their potentially severe consequences. Vaccines stimulate the body’s immune system to recognize and respond effectively to specific pathogens. As a result, immunization has profoundly impacted global health by reducing morbidity, mortality, and disability associated with infectious diseases[1].
Vaccines have successfully eradicated or significantly reduced the incidence of several deadly diseases, such as smallpox, and have played a crucial role in controlling and eliminating others, including polio and measles[2]. They have also prevented complications and long-term sequelae associated with infections, such as pneumonia, meningitis, and certain cancers[1].
Parents’ knowledge about immunization is pivotal, as they are the primary decision-makers for their children’s healthcare. Understanding parents’ knowledge is crucial for public health interventions, policy development, and designing effective communication strategies to improve immunization rates. Knowledge empowers parents to make informed decisions regarding their children’s immunizations. It enables them to understand vaccines’ benefits, risks, and importance in protecting their child's health and well-being[3].
Knowledge gaps and misconceptions are a few factors contributing to vaccine hesitancy, defined as the delay or refusal of vaccination despite the availability of vaccines. Parents who lack accurate knowledge may hold unfounded beliefs about vaccine safety, effectiveness, or necessity. Addressing these knowledge gaps is essential to mitigate vaccine hesitancy and promote vaccine confidence[4]. Studies have shown that enhancing parents’ knowledge increases vaccine acceptance and reduces hesitancy[5,6]. Health literacy is obtaining, understanding, and applying health information to make informed decisions. Parents with higher health literacy levels are better equipped to comprehend immunization-related information and navigate healthcare systems effectively[7]. Vaccine hesitancy among parents is a multifaceted issue influenced by a spectrum of factors, including misinformation, religious beliefs, and concerns about vaccine safety and necessity. Studies have demonstrated varying parental knowledge about immunization, significantly impacting public health[8]. For instance, Matta et al.[9] revealed that 41.4% of parents needed better knowledge about vaccination. At the same time, Alshammari et al.[10] reported a more promising scenario, with 73.3% of parents exhibiting good knowledge of childhood immunization.
Despite these variations, there is a clear trend of apprehension and reluctance towards vaccination in certain groups. Facciolà et al.[11] highlighted that low vaccination coverage rates for vaccines such as pneumococcal and HPV suggest that many parents may not be fully informed about immunization schedules. This lack of awareness, coupled with the 91.5% of parents who cite fear of side effects as a deterrent to vaccination, underscores widespread misconceptions about vaccine safety. Such concerns are pivotal contributors to the hesitancy that hinders achieving optimal immunization coverage[11].
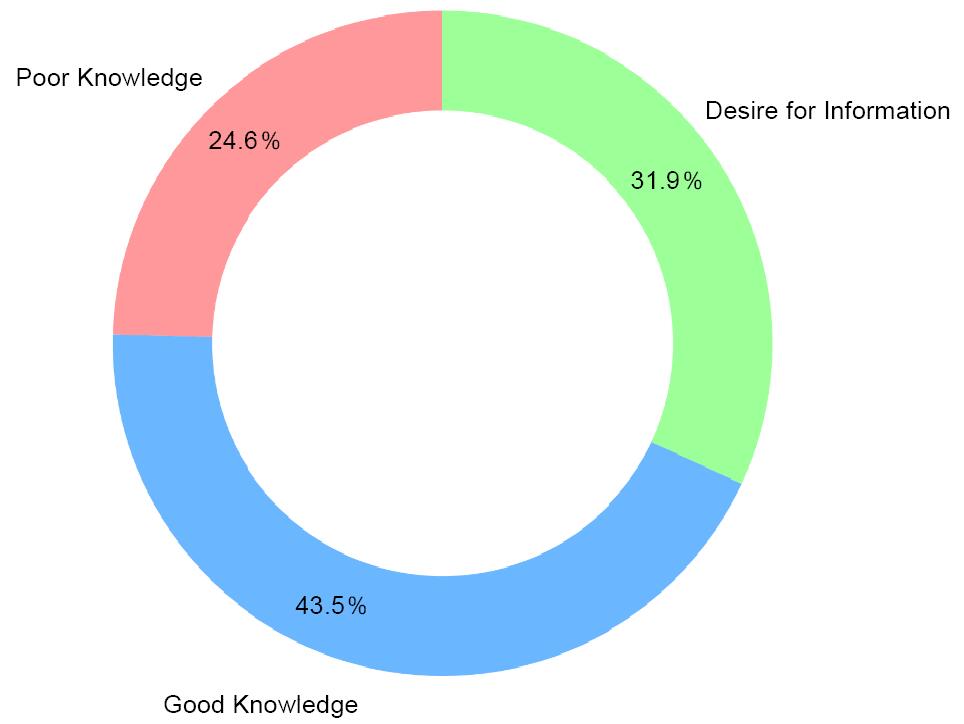
Adding to the issue’s complexity, Bianco et al.[12] found that 7.7% of parents were hesitant about vaccines, as measured by the PACV score, with a considerable 24.6% delaying or refusing at least one dose for their child. The study suggests that vaccine hesitancy is exacerbated by misinformation, notably through mass media, and a skeptical view of vaccinations as a commercial ploy rather than a public health necessity.
In aligning these findings, the work of Paterson et al.[13] further underscores the urgent need for strategic communication efforts that address the various sources of vaccine hesitancy to promote informed decision-making among parents. Moreover, Napolitano et al.[14] identified a pressing need for enhanced communication strategies that effectively bridge the information gap, as indicated by the 31.9% of parents who expressed a desire for additional information about vaccines (Figure 1).
|
Figure 1. Parental knowledge and desire for information on vaccination.
Ultimately, these studies collectively emphasize the necessity for healthcare providers to develop trust-building and effective communication strategies that deliver transparent and accurate information about vaccines and address specific parental concerns. This approach is crucial in strengthening the public’s confidence in immunization programs and ensuring their trust in healthcare recommendations.
2 METHODS
Studies published between 2018 and 2023 were identified through searches in PubMed, Scopus, and Embrace research databases, as they contained full-text articles. The search was conducted using keywords such as “parents’ knowledge or understanding of immunization”, “vaccine-preventable diseases”, “vaccine safety”, “vaccine schedules”, or “the benefits of immunization”. The inclusion criteria were studies written in English or Arabic, focusing on parents or caregivers of children (infants, toddlers, and school-aged children). Studies including parents of children with special healthcare needs or from diverse socioeconomic backgrounds were also considered. Various study designs were included, such as cross-sectional surveys, cohort studies, randomized controlled trials, qualitative interviews, or mixed-methods approaches. If the full text was available, the study was included.
2.1 Search Outcome
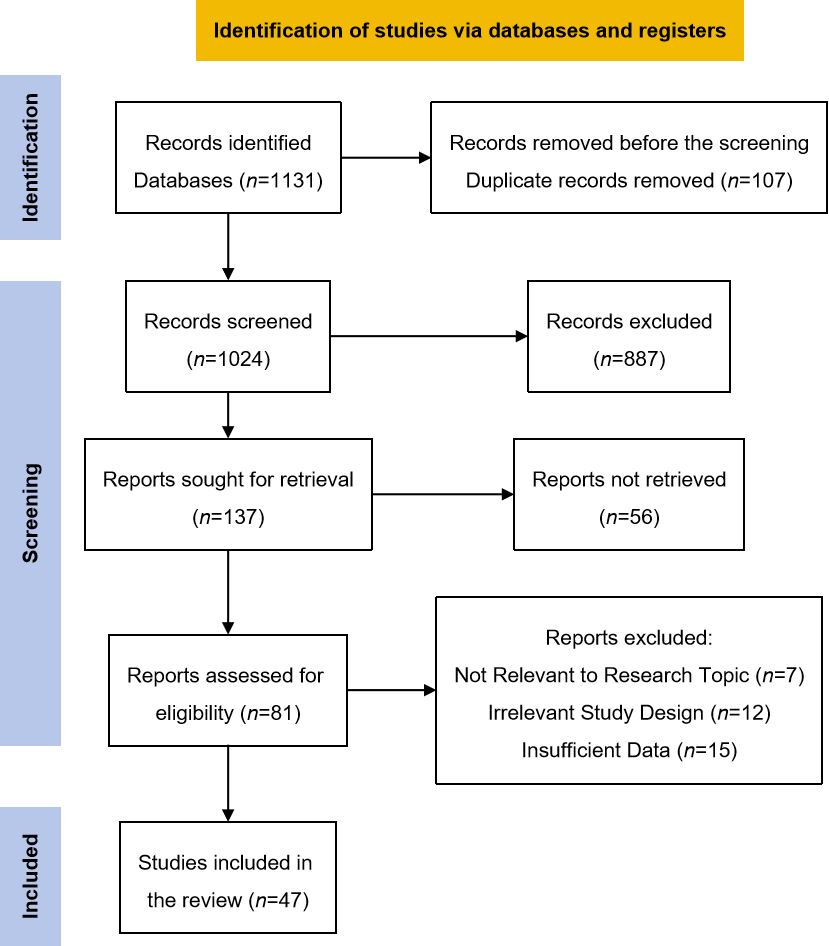
During the search, 137 studies were found, all in English and none in Arabic. All 137 studies were assessed against the criteria for inclusion. The researchers of the current review selected the studies by reading their abstracts, and in some cases, the entire paper was required to determine if the study met the inclusion criteria (Figure 2). Out of the total studies, 109 studies that did not meet the criteria were excluded, which left 47 research studies summarized in Supplementary Table 1.
|
Figure 2. PRISMA flow diagram for review selection.
2.2 Data Abstraction
From the 47 chosen studies, the following information was taken into Supplementary Table 1: The study’s purpose, theoretical framework, country, sample size, design, primary findings, and the author(s) and year of publication.
3 RESULTS
3.1 Characteristics of the Reviewed Studies
Out of the 47 articles reviewed, Table 1 provides a comprehensive breakdown of the research methodologies used to investigate parents’ knowledge regarding childhood immunization. Twenty-seven articles utilized quantitative surveys to gather data, which provided structured and numeric insights into parental knowledge and attitudes. This approach sheds light on the diverse approaches used by researchers. In parallel, eight articles opted for qualitative interviews or focus groups, delving deeper into parents’ subjective experiences and perceptions. The synergy of quantitative and qualitative methods was evident in 5 articles that embraced mixed-methods approaches, offering a more holistic understanding of the subject matter. Lastly, four articles contributed to the body of knowledge through systematic reviews and meta-analyses, synthesizing existing research to draw overarching conclusions. The various research methodologies used in this study emphasize the complex nature of the topic. They demonstrate the necessity for a diverse range of investigative techniques to address parents’ knowledge of childhood immunization comprehensively. Additionally, Table 1 provides an overview of the research methodologies used in the reviewed articles.
Table 1. The Research Methodologies Used in the Reviewed Articles
Research Methodology |
Number of Reviewed Articles |
Quantitative surveys |
27 |
Qualitative interviews / Focus groups |
8 |
Mixed-methods approaches |
5 |
Systematic reviews / Meta-analyses |
7 |
Supplementary Table 1 comprises a collection of 47 studies, each contributing unique insights into the complex landscape of vaccine hesitancy, vaccine knowledge, and immunization practices. These studies span various countries and regions, shedding light on the factors influencing vaccination decisions. Among the studies, India and the USA are the most frequently explored countries, each represented by multiple studies delving into vaccine hesitancy and acceptance in different contexts. Additionally, there is a diverse array of studies from various other countries, including Jordan, Hungary, Switzerland, Bosnia, Italy, Canada, Australia, the United Kingdom, Georgia, Poland, Lithuania, Greece, Malaysia, Indonesia, and Pakistan, collectively providing a global perspective on vaccination challenges.
Regarding research design, the studies in this table employ a range of methodologies. Most cross-sectional studies investigate vaccine hesitancy and knowledge among specific populations. There are also qualitative studies, narrative reviews, policy papers, and systematic reviews, each offering valuable insights into the multifaceted nature of vaccine-related issues.
Sample sizes in these studies exhibit variability, reflecting the diversity of research objectives. The largest sample size was observed in a study conducted in the United States involving 1,180 women surveyed to understand their views on COVID-19 vaccination during pregnancy. In contrast, the smallest sample size is from a qualitative study conducted in Pakistan, where 38 mothers and 40 fathers participated in 12 focus groups discussing breastfeeding practices. These varying sample sizes highlight the adaptability of research methods to address specific research questions effectively.
Within this compilation of studies, there are two review papers and two systematic reviews. These comprehensive reviews provide in-depth analyses of vaccine hesitancy, communication strategies, and knowledge gaps in different regions. By synthesizing existing research, these reviews offer a consolidated understanding of the challenges and potential solutions related to vaccination.
3.2 Parents’ Knowledge regarding Immunization
Parents’ understanding of the concept of immunization is crucial in shaping their decision-making process when it comes to vaccinating their children. Research indicates that parents’ knowledge and understanding of immunization vary widely. While many parents understand vaccines and their role in preventing diseases, there are still notable gaps in knowledge and persistent misconceptions. When it comes to vaccine-preventable diseases, parents generally possess a reasonable understanding, especially for diseases that have high public awareness, such as measles, polio, and pertussis (whooping cough)[15]. They are often aware of the potential severity and complications associated with these diseases, which motivates them to vaccinate their children to protect them from these preventable illnesses[16].
Regarding vaccine safety, parents’ understanding can vary. Some studies have shown that parents generally express confidence in the safety of vaccines and trust the regulatory systems in place to ensure their safety. In addition, they understand that vaccines undergo rigorous testing and are continually monitored for adverse events[17,18]. However, it is essential to note that a subset of parents may have concerns or misconceptions regarding vaccine safety. These concerns may be related to specific vaccine ingredients, such as thimerosal, or a perceived link between vaccines and adverse events. Such concerns can contribute to vaccine hesitancy and may significantly impact parents’ decision-making[19,20].
Regarding vaccine efficacy, parents typically recognize the effectiveness of vaccines in preventing diseases. In addition, they understand that vaccines can substantially reduce the risk of contracting vaccine-preventable diseases and their associated complications. This knowledge is a positive factor in their decision to vaccinate their children[6,21]. Despite these general understandings, studies consistently identify knowledge gaps and misconceptions about vaccines and immunization. For example, parents may lack specific knowledge regarding vaccine schedules, the number of doses required, or the need for booster shots. They may also have limited knowledge about less common vaccine-preventable diseases or vaccines less prominently discussed in public health campaigns[11,22].
Additionally, misconceptions about vaccines and their effects may persist. For example, some parents may believe that vaccines weaken the immune system, cause autism, or lead to long-term health problems. These misconceptions often stem from misinformation on the internet, social media, or anecdotal stories shared within their social networks[6,19,23].
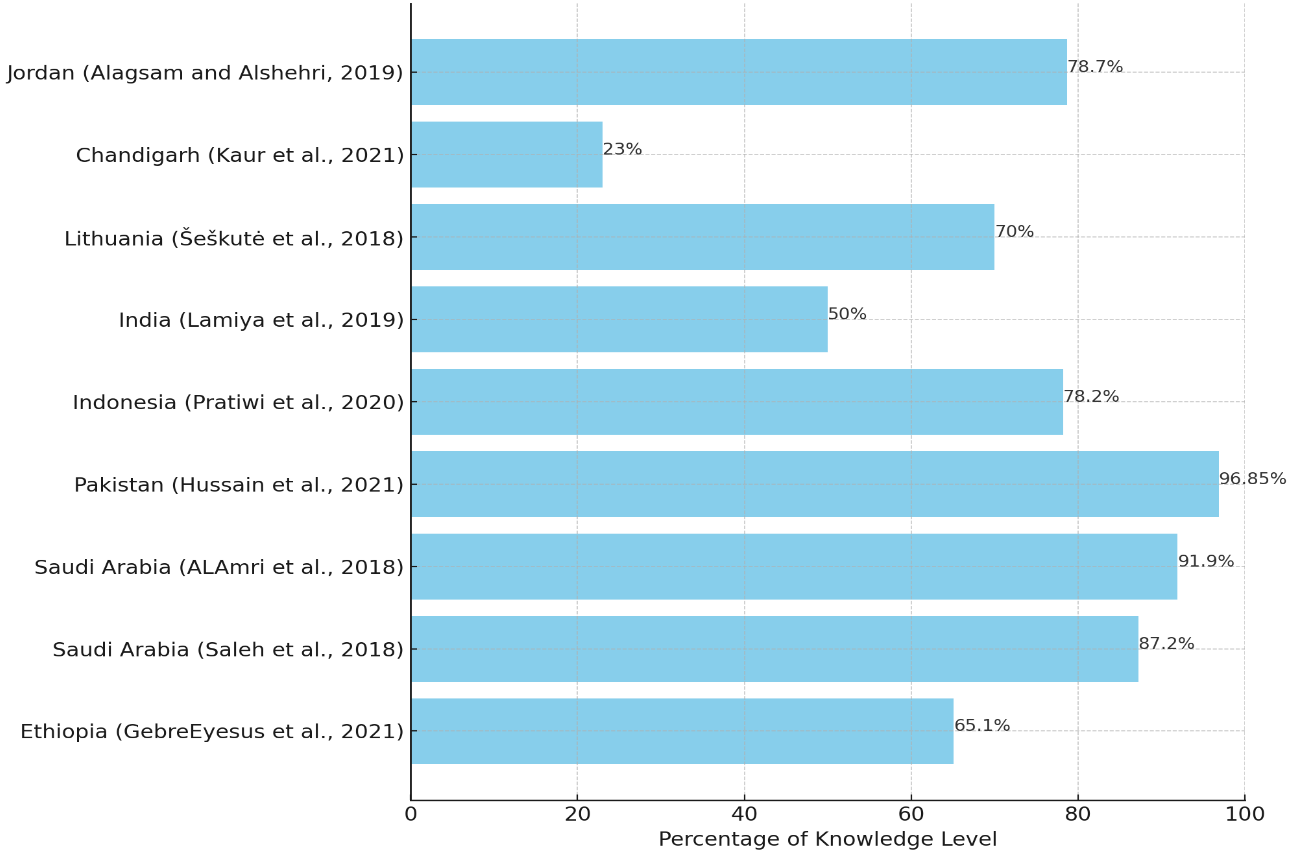
The global analysis of parental knowledge and attitudes toward immunization sets the stage for a more detailed examination of the levels of awareness across various regions. Transitioning from a general overview to individual studies, we observe the nuances in parents’ knowledge of vaccines. This shift from global to localized insights underlines the importance of recognizing how various educational backgrounds and socio-economic circumstances contribute to the varied levels of understanding about immunization practices among parents (Figure 3).
|
Figure 3. Parental knowledge levels on child vaccination: Comparative analysis by country and study.
GebreEyesus et al.[24] from Ethiopia found that while 65.1% of parents understood infant immunization well, this knowledge needed to be more consistent across all groups. Parents who lived in cities and had more education understood immunization practices better. In Saudi Arabia, Habibl et al.[25] found that 87.2% of parents displayed positive attitudes and practices towards vaccination, suggesting a high level of awareness. ALAmri et al.[26], on the other hand, showed that while most parents (91.9%) knew what vaccinations were for, only 41.6% knew what multiple doses meant, and only 37.1% knew that giving a child multiple vaccines at the same time does not hurt their immunity.
In Pakistan, Hussain et al.[27] showed that knowledge was significantly better among parents with higher education, with 96.85% recognizing the importance of vaccination. Despite this, economic factors were a concern, with more than half (57.58%) indicating that vaccine affordability was a principal factor in delays in immunization. Pratiwi et al.[28] found a commendable average knowledge score of 78.2 out of 100 among parents regarding rotavirus in Indonesia. However, only 31.6% knew the vaccine's exclusion from the national health insurance program.
In India, Lamiya et al.[29] reported relatively fair vaccine knowledge. However, the specifics of individual vaccines were less known, with a notable lack of detailed understanding that needs to be addressed through targeted education. The Lithuanian study by Šeškutė et al.[30] revealed that while most mothers were aware of vaccine-preventable diseases, their knowledge about the efficacy and safety of vaccines themselves was less comprehensive.
In Chandigarh, Kaur et al.[31] found that although most mothers knew about vaccination needs and schedules, they needed to learn more about them. This affected total immunization rates, as only 23% of children in nonmigratory populations were fully immunized. Lastly, Alagsam and Alshehri[32] in Jordan reported that despite 78.7% of parents understanding the value of vaccines for child health, a significant portion (83%) still had concerns about vaccine safety.
These statistics reinforce the need for tailored health education programs that increase the percentage of parents with comprehensive vaccine knowledge and address the persistent gaps and misconceptions about vaccine safety and schedules. It is clear that educational attainment is a strong predictor of vaccine knowledge, and as such, interventions should focus on demystifying vaccinations for parents across all educational backgrounds.
3.3 Factors Influencing Parents’ Knowledge and Willingness
Socio-demographic factors, such as age, education, and income, significantly shape parents’ knowledge about immunization. Research has consistently shown associations between these factors and parents’ level of understanding. For example, age can influence parents’ knowledge, with younger parents often exhibiting higher levels of knowledge due to growing up with greater exposure to vaccination campaigns and educational materials. Conversely, older parents may have experienced vaccination in a different era, potentially leading to gaps in their knowledge regarding newer immunization practices[33,34]. In addition, education has been consistently linked to better knowledge and understanding of immunization. Parents with higher levels of education tend to have greater access to information, possess critical thinking skills, and demonstrate the ability to understand scientific concepts.
Consequently, they are better equipped to comprehend the benefits and safety of vaccines[35]. Socio-economic status, often measured by income, has also been identified as influencing parents’ knowledge. Studies have shown that higher-income parents have greater access to healthcare resources, including reliable immunization information. This increased access can contribute to a better understanding of vaccination and its importance[36].
This research compilation provides a comprehensive yet coherent perspective, which aligns with the notion that socio-demographic factors are closely linked to parental awareness about immunization. These studies confirm and extend the previously discussed factors, such as age, education, and income, and their impact on parental comprehension of vaccinations. For instance, Abdullah et al.[37] pinpointed that factors such as the age of the last child, absence of tertiary education, and information sources, such as non-healthcare providers, are predictors for inadequate knowledge among Malaysian parents. Lewandowska et al.[38] echoed the role of misinformation, adding that general practitioners are pivotal in shaping vaccination decisions, suggesting that the medical community’s endorsement or skepticism can greatly influence parental attitudes. Goss et al.[39] similarly found that parents’ knowledge about the vaccine’s efficacy and safety correlates with their decision to vaccinate against influenza. Napolitano et al.[40] highlighted the importance of healthcare professionals in disseminating information, as parents who cited physicians as their information source showed higher awareness and vaccination rates against rotavirus in Italy. In Greece, Giannakou et al.[41] found that pediatricians significantly impact mothers’ decisions to vaccinate their children and that mothers with more education know much more about vaccines. Lastly, Ganczak et al.[42] uncovered a willingness to vaccinate against HPV in Poland despite limited specific knowledge about the virus, emphasizing the need for targeted educational interventions.
Cultural and religious beliefs play a significant role in shaping parents’ knowledge and decision-making regarding immunization. Different cultural and religious perspectives can influence beliefs about health, illness, and preventive measures like vaccination. Cultural beliefs can shape parents’ knowledge by influencing their understanding of disease causation, prevention, and treatment. For example, cultural beliefs regarding the body’s natural ability to fight off illness or the use of traditional healing practices may impact parents’ perceptions of the need for vaccination[43]. Religious beliefs also play a role in parents’ knowledge about immunization. Some religious communities may have specific vaccine beliefs or concerns, leading to vaccine knowledge and acceptance variations. For instance, certain religious groups may have religious exemptions or reservations about specific vaccine components[44]. Sources of information and media influence significantly impact parents’ knowledge about immunization. The information parents receive and the sources they rely on can shape their understanding and decision-making. Healthcare providers are considered important sources of information for parents. Effective communication and clear recommendations from healthcare providers can positively influence parents’ knowledge and attitudes toward immunization. Parents who perceive healthcare providers as trustworthy and knowledgeable are more likely to rely on their recommendations and accurate information[45,46]. Media, including traditional and social media platforms, play a significant role in shaping parents’ knowledge. Misinformation, rumors, and vaccine-related controversies can spread rapidly through social media, leading to misconceptions and vaccine hesitancy. The impact of media on parents’ knowledge highlights the importance of promoting accurate and evidence-based information through reliable sources and countering misinformation[47].
Healthcare provider communication and recommendations significantly influence parents’ knowledge about immunization. Clear and effective communication from healthcare providers can positively impact parents’ understanding and decision-making. Studies have shown that parents who have open and informative discussions with healthcare providers are more likely to have accurate knowledge about vaccines and their benefits. Effective provider communication can address parents’ concerns, provide vaccine-related information, and clarify misconceptions. Such interactions are crucial in improving parents’ knowledge and vaccine acceptance[48,49].
Vaccine hesitancy is when parents delay or refuse vaccines despite their availability. This behavior is mainly due to gaps in knowledge and concerns or misconceptions about immunization. Studies have shown that vaccine-hesitant parents usually have lower knowledge about vaccines. They also harbor misconceptions about vaccine safety and effectiveness. Therefore, addressing these knowledge gaps and misconceptions is crucial to combat vaccine hesitancy. Accurate information is necessary to enhance parents’ knowledge and promote immunization[50].
4 DISCUSSION
The discussion surrounding parents’ knowledge about immunization has yielded several significant findings. There is apparent variability in parents’ understanding of immunization, with a combination of accurate knowledge and persistent knowledge gaps and misconceptions. Although many parents have a basic comprehension of vaccines and their function in preventing diseases, there are still areas where their knowledge can be enhanced.
Parents typically possess a reasonable understanding of vaccine-preventable diseases, particularly those with high public awareness. They are also acquainted with the potential severity and complications of contracting such diseases, which motivates them to vaccinate their children and protect them from these preventable illnesses. This corresponds with the perceived susceptibility and severity in health behavior models, where individuals are more likely to take preventive measures when they perceive themselves or their children at risk[15].
However, there is some variability in parents’ understanding regarding vaccine safety. While many express confidence in the safety of vaccines and trust the regulatory systems in place, a subset of parents may have concerns or misconceptions. These concerns may be related to specific vaccine ingredients or a perceived link between vaccines and adverse events. Addressing these concerns and providing accurate information is crucial to alleviating vaccine hesitancy and promoting informed decision-making[18,31]. Regarding vaccine efficacy, parents generally recognize the effectiveness of vaccines in preventing diseases. In addition, they understand that vaccines can substantially reduce the risk of contracting vaccine-preventable diseases and their associated complications. This knowledge is a positive factor in their decision to vaccinate their children[6,21]. Although there is a general understanding of vaccines and immunization, some notable knowledge gaps and misconceptions remain. Some people may not have enough information about less common vaccine-preventable diseases or vaccines not prominently discussed in public health campaigns. These knowledge gaps can affect the completeness and timeliness of immunization, as per research[11,22].
Furthermore, misconceptions about vaccines and their effects may persist among some parents. For example, beliefs that vaccines weaken the immune system and cause autism or lead to long-term health problems can contribute to vaccine hesitancy and decision-making based on misinformation. Addressing these misconceptions and providing accurate information is essential to promoting informed decision-making[6,19,23]. Reflecting on these findings, it is clear that efforts to enhance parents’ knowledge about immunization are critical. Providing accurate information, education, and effective communication strategies are essential to addressing knowledge gaps and misconceptions. Healthcare providers and public health authorities are pivotal in ensuring parents have access to reliable information and are equipped with the necessary knowledge to make informed decisions about their children's immunization.
4.1 Implications and Recommendations
The findings discussed have several implications for practice and policy to enhance parents’ knowledge regarding immunization.
4.2 Strengthening Healthcare Provider Communication
Healthcare providers should have practical communication skills to engage with parents and address their knowledge gaps and concerns. This involves active listening, using clear and understandable language, and providing evidence-based information tailored to individual parents’ needs. Enhancing provider communication can positively influence parents’ knowledge and decision-making.
4.3 Targeted Educational Interventions
Tailored educational interventions should be developed and implemented to address specific knowledge gaps and misconceptions identified in different populations. These interventions should consider cultural, linguistic, and literacy needs to enhance understanding and promote informed decision-making. In addition, educational programs can utilize various formats, such as workshops, seminars, and informational materials, to effectively disseminate accurate information and debunk misconceptions.
4.4 Regulation of Online Information
Media and online platforms significantly impact parents’ knowledge about vaccines. Therefore, it is crucial to regulate and counteract vaccine misinformation. Public health authorities and policymakers should collaborate with technology companies and social media platforms to promote accurate information and implement fact-checking mechanisms. Additionally, monitoring and addressing vaccine-related misinformation should be a top priority to ensure parents have access to reliable vaccine information.
4.5 Collaboration with Community Stakeholders
Engaging community stakeholders, including religious and cultural leaders, can help address specific beliefs and concerns surrounding immunization. Building partnerships and involving community members in developing and implementing educational programs can foster trust, improve information dissemination, and address cultural and religious perspectives.
4.6 Longitudinal Research and Evaluation
Longitudinal studies tracking parents’ knowledge over time can provide insights into the stability and changes in knowledge levels and their impact on vaccine acceptance. Evaluating the effectiveness of interventions and strategies to improve parents’ knowledge is crucial to inform evidence-based practices and identify areas for improvement.
5 CONCLUSION
Drawing from the rigor of 47 studies, the emerging conclusion is robust and evidence-based: Parental knowledge is an essential driver for the success of immunization programs. The collective findings reveal a dual reality where, despite widespread recognition of the critical role of vaccines in disease prevention, there are persistent and significant gaps in parental understanding. These gaps extend to the safety and scheduling of vaccines and a comprehensive grasp of all vaccine-preventable diseases. Moreover, pervasive myths and misconceptions - notably those linking vaccines to autism - continue to exert a detrimental impact on vaccination efforts.
The reviews underscore a range of factors influencing parental knowledge and attitudes. Socio-demographic elements such as educational level, socio-economic status, and urban versus rural residency markedly affect parental vaccination awareness and decisions. The influence of healthcare providers, particularly pediatricians, emerges as a potent factor in shaping parental perceptions and actions. Misinformation, particularly that propagated online, has been identified as a significant contributor to vaccine hesitancy, suggesting a need for stringent monitoring and correction of health information disseminated to the public.
Research suggests adopting a multi-faceted approach to address the issues related to vaccine hesitancy. This approach includes regulating online information to combat misinformation and engaging with community and religious leaders who can help bridge the gap between cultural beliefs and scientific evidence.
Targeting these influencing factors through specific interventions makes it possible to significantly increase parental knowledge, which is crucial for enhancing vaccine acceptance and uptake. Healthcare authorities and providers must prioritize communication strategies tailored to address the identified gaps and misconceptions. Efforts that equip parents with accurate, comprehensive information will lead to more informed decisions, ultimately bolstering immunization rates and fortifying community health against vaccine-preventable diseases.
Acknowledgements
Not applicable.
Conflicts of Interest
The authors declared no conflict of interest.
Author Contribution
Ayoub MY and Al-Ghabeesh S conceived and designed the paper, developed the methodology, interpreted the data, contributed reagents, materials, and analysis tools or data. All authors contributed to the manuscript and approved the final version.
References
[1] Switzerland. World Health Organization. WHO train the trainer workshop: developing national deployment and vaccination plans (NDVP) for pandemic influenza vaccines. Accessed 11 September 2019. Available at:[Web]
[2] Tappero JW, Cassell CH, Bunnell RE et al. US Centers for Disease Control and Prevention and Its Partners’ Contributions to Global Health Security. Emerg Infect Dis, 2017; 23: S5-S14.[DOI]
[3] Reich JA. Vaccine Refusal and Pharmaceutical Acquiescence: Parental Control and Ambivalence in Managing Children’s Health. Am Sociol Rev, 2020; 85: 106-127.[DOI]
[4] Agrawal A, Kolhapure S, Di Pasquale A et al. Vaccine Hesitancy as a Challenge or Vaccine Confidence as an Opportunity for Childhood Immunisation in India. Infect Dis Ther, 2020; 9: 421-432.[DOI]
[5] Hasnan S, Tan NC. Multi-domain narrative review of vaccine hesitancy in childhood. Vaccine, 2021; 39: 1910-1920.[DOI]
[6] Olson O, Berry C, Kumar N. Addressing Parental Vaccine Hesitancy towards Childhood Vaccines in the United States: A Systematic Literature Review of Communication Interventions and Strategies. Vaccines, 2020; 8: 590.[DOI]
[7] Lorini C, Santomauro F, Donzellini M et al. Health literacy and vaccination: A systematic review. Hum Vaccines, 2018; 14: 478-488.[DOI]
[8] Deml MJ, Buhl A, Notter J et al. “Problem patients and physicians’ failures”: What it means for doctors to counsel vaccine hesitant patients in Switzerland. Soc Sci Med, 2020; 255: 112946.[DOI]
[9] Matta P, El Mouallem R, Akel M et al. Parents’ knowledge, attitude and practice towards children’s vaccination in Lebanon: role of the parent-physician communication. BMC Public Health, 2020; 20: 1439.[DOI]
[10] Alshammari SZ, AlFayyad I, Altannir Y et al. Parental Awareness and Attitude about Childhood Immunization in Riyadh, Saudi Arabia: A Cross-Sectional Study. Int J Environ Res Public Health, 2021; 18: 8455.[DOI]
[11] Facciolà A, Visalli G, Orlando A et al. Vaccine Hesitancy: An Overview on Parents’ Opinions about Vaccination and Possible Reasons of Vaccine Refusal. J Public Health Res, 2019; 8: 1436.[DOI]
[12] Bianco A, Mascaro V, Zucco R et al. Parent perspectives on childhood vaccination: How to deal with vaccine hesitancy and refusal?. Vaccine, 2019; 37: 984-990.[DOI]
[13] Paterson P, Chantler T, Larson HJ. Reasons for non-vaccination: Parental vaccine hesitancy and the childhood influenza vaccination school pilot programme in England. Vaccine, 2018; 36: 5397-5401.[DOI]
[14] Napolitano F, D’Alessandro A, Angelillo IF. Investigating Italian parents’ vaccine hesitancy: A cross-sectional survey. Hum Vaccines, 2018; 14: 1558-1565.[DOI]
[15] Goldenberg MJ. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science. In: Science, Values, and the Public. University of Pittsburgh Press: Pennsylvania, USA, 2021.
[16] Attwell K, Navin M. Childhood Vaccination Mandates: Scope, Sanctions, Severity, Selectivity, and Salience. Milbank Q, 2019; 97: 978-1014.[DOI]
[17] Musa S, Kulo A, Habersaat KB et al. A qualitative interview study with parents to identify barriers and drivers to childhood vaccination and inform public health interventions. Hum Vaccines, 2021; 17: 3023-3033.[DOI]
[18] Skirrow H, Barnett S, Bell S et al. Women’s views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: a multi-methods study in the UK. BMC Pregnancy Childb, 2022; 22: 33.[DOI]
[19] Gabis LV, Attia OL, Goldman M et al. The myth of vaccination and the autism spectrum. Eur J Paediatr Neuro, 2022; 36: 151-158.[DOI]
[20] Geoghegan S, O’Callaghan KP, Offit PA. Vaccine Safety: Myths and Misinformation. Front Microbiol, 2020; 11: 372.[DOI]
[21] McDonald P, Limaye RJ, Omer SB et al. Exploring California’s new law eliminating personal belief exemptions to childhood vaccines and vaccine decision-making among homeschooling mothers in California. Vaccine, 2019; 37: 742-750.[DOI]
[22] Verulava T, Jaiani M, Lordkipanidze A et al. Mothers’ Knowledge and Attitudes Towards Child Immunization in Georgia. Open Public Health J, 2019; 12: 232-237.[DOI]
[23] Mendel-Van Alstyne JA, Nowak GJ et al. What is ‘confidence’ and what could affect it?: A qualitative study of mothers who are hesitant about vaccines. Vaccine, 2018; 36: 6464-6472.[DOI]
[24] GebreEyesus FA, Tarekegn TT, Amlak BT et al. Knowledge, Attitude, and Practices of Parents About Immunization of Infants and Its Associated Factors in Wadla Woreda, North East Ethiopia, 2019. Pediatr Health Med Ther, 2021; 12: 223-238.[DOI]
[25] Habibl RF, Alsubhil RA, Saadawi DW et al. Assessment of Knowledge, Attitude and Practice of Parents Towards Immunization of Children in Saudi Arabia, 2018. Egypt J Hosp Med, 2018; 71: 2585-2589.[DOI]
[26] ALAmri ES, Horaib YF, Alanazi WR. Knowledge and Attitudes of Parents on Childhood Immunization in Riyadh, Saudi Arabia. Egypt J Hosp Med, 2018; 70: 251-256.[DOI]
[27] Hussain A, Zahid A, Malik M et al. Assessment of Parents’ Perceptions of Childhood Immunization: A Cross-Sectional Study from Pakistan. Children-Basel, 2021; 8: 1007.[DOI]
[28] Pratiwi AD, Endarti D, Andayani T et al. Parent’s Knowledge on Rotavirus Diarrhea and Vaccine in Indonesia. Vaccine Research, 2020; 7: 38-43.
[29] Lamiya KK, Mundodan JM, Haveri SP. Knowledge, attittude and practice among mothers of under five children on immunization. Int J Community Med Public Health, 2019; 6: 1252-1257.[DOI]
[30] Šeškutė M, Tamulevičienė E, Levinienė G. Knowledge and Attitudes of Postpartum Mothers towards Immunization of Their Children in a Lithuanian Tertiary Teaching Hospital. Medicina, 2018; 54: 2.[DOI]
[31] Kaur R, Jassal D, Sharma N et al. Knowledge, attitude, and practice of mothers regarding immunization. Indian J Pharmacol, 2021; 53: 336-338.
[32] Alagsam EH, Alshehri AA. Knowledge, attitude, and practice of parents on childhood immunization schedule in Saudi Arabia. Int J Med Dev C, 2019; 3: 457-461.[DOI]
[33] Alsulaiman JW, Mazin M, Al-Shatanawi TN et al. Parental Willingness to Vaccinate Their Children Against SARS-CoV-2 in Jordan: An Explanatory Cross-Sectional Study. Risk Manag Healthc P, 2022; 955-967.[DOI]
[34] Tran CL, Selewski DT, Oh GJ et al. Pediatric Immunization Practices in Nephrotic Syndrome: An Assessment of Provider and Parental Knowledge. Front Pediatr, 2021; 8: 619548.[DOI]
[35] Guzman-Holst A, DeAntonio R, Prado-Cohrs D et al. Barriers to vaccination in Latin America: A systematic literature review. Vaccine, 2020; 38: 470-481.[DOI]
[36] Voo JYH, Lean QY, Ming LC et al. Vaccine Knowledge, Awareness and Hesitancy: A Cross Sectional Survey among Parents Residing at Sandakan District, Sabah. Vaccines, 2021; 9: 1348.[DOI]
[37] Abdullah AC, Manaf RA, Zulkefl NAM. Predictors For Inadequate Knowledge And Negative Attitude Towards Childhood Immunization Among Parents In Hulu Langat, Selangor, Malaysia. Malaysian J Public Health Med, 2018; 18: 102-112.
[38] Lewandowska A, Lewandowski T, Rudzki G et al. Opinions and Knowledge of Parents Regarding Preventive Vaccinations of Children and Causes of Reluctance toward Preventive Vaccinations. Int J Environ Res Public Health, 2020; 17: 3694.[DOI]
[39] Goss MD, Temte JL, Barlow S et al. An assessment of parental knowledge, attitudes, and beliefs regarding influenza vaccination. Vaccine, 2020; 38: 1565-1571.[DOI]
[40] Napolitano F, Ali Adou A, Vastola A et al. Rotavirus Infection and Vaccination: Knowledge, Beliefs, and Behaviors among Parents in Italy. Int J Environ Res Public Health, 2019; 16: 1807.[DOI]
[41] Giannakou K, Kyprianidou M, Hadjikou A et al. Knowledge of mothers regarding children's vaccinations in Greece: an online cross-sectional study. BMC Public Health, 2021; 21: 2119.[DOI]
[42] Ganczak M, Owsianka B, Korzeń M. Factors that Predict Parental Willingness to Have Their Children Vaccinated against HPV in a Country with Low HPV Vaccination Coverage. Int J Environ Res Public Health, 2018; 15: 645.[DOI]
[43] Zakar R, Zakar MZ, Zaheer L et al. Exploring parental perceptions and knowledge regarding breastfeeding practices in Rajanpur, Punjab Province, Pakistan. Int Breastfeed J, 2018; 13: 24.[DOI]
[44] Krok‐Schoen JL, Bernardo BM, Weier RC et al. Belief About Mandatory School Vaccinations and Vaccination Refusal Among Ohio Appalachian Parents: Do Demographic and Religious Factors, General Health, and Political Affiliation Play a Role?. J Rural Health, 2018; 34: 283-292.[DOI]
[45] Ashkenazi S, Livni G, Klein A et al. The relationship between parental sources of information and knowledge about measles / measles vaccine and vaccine hesitancy. Vaccine, 2020; 38: 7292-7298.[DOI]
[46] Shen SC, Dubey V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can Fam Physician, 2019; 65: 175-181.
[47] Steffens MS, Dunn AG, Wiley KE et al. How organizations promoting vaccination respond to misinformation on social media: a qualitative investigation. BMC Public Health, 2019; 19: 1348.[DOI]
[48] Dempsey AF, O’Leary ST. Human Papillomavirus Vaccination: Narrative Review of Studies on How Providers’ Vaccine Communication Affects Attitudes and Uptake. Acad Pediatr, 2018; 18: S23-S27.[DOI]
[49] Huber A, Gazder J, Dobay O et al. Attitudes towards varicella vaccination in parents and pediatric healthcare providers in Hungary. Vaccine, 2020; 38: 5249-5255.[DOI]
[50] Yufika A, Wagner AL, Nawawi Y et al. Parents’ hesitancy towards vaccination in Indonesia: A cross-sectional study in Indonesia. Vaccine, 2020; 38: 2592-2599.[DOI]
Copyright © 2024 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.





 Copyright ©
Copyright ©