Application of Early Multi-dimensional Cardiac Rehabilitation Nursing in Percutaneous Coronary Intervention and Its Effects on Adverse Events and Patients’ Adherence to Medication
Surui Zhao1*, Huan Xu1, Fang Liu2, Xuemin Guo1, Yonglou Zhang1
1Department of Cardiology Ⅳ, Cangzhou Central Hospital, Hebei Province, China
2Department of Cardiology II, Cangzhou Central Hospital, Hebei Province, China
*Correspondence to: Surui Zhao, Department of Cardiology Ⅳ, Cangzhou Central Hospital, No.16 West Xinhua Road, Yunhe District, Hebei Province 061000, China; Email: 724074661@qq.com
Abstract
Objective: To evaluate the application value of early multi-dimensional cardiac rehabilitation nursing in percutaneous coronary intervention (PCI) and its effects on adverse events and patients’ adherence to medication.
Methods: A total of 90 patients that underwent PCI in our hospital from January 2019 to January 2020 were selected as the study subjects. The patients were divided into two groups according to the order of admission, the control group and the study group, with 45 patients in each group. Patients in the control group were cared for using conventional nursing methods, while those in the study group were cared for using conventional nursing methods combined with early multi-dimensional cardiac rehabilitation nursing. The efficacy of nursing and the incidence of adverse events in the two groups of patients were assessed and compared. The exercise of self care agency scale (ESCA) was used to evaluate the self-care ability of patients after intervention. The generic quality of life inventory-74 (GQOLI-74) was used to assess the patients’ quality of life after intervention. The Morisky medication adherence scale 9 (MMAS-8) was used to assess the patients’ adherence to medication before and after intervention. The hospital anxiety and depression scale (HAD) was used to assess the patients’ emotional state before and after intervention.
Results: The total nursing satisfaction after intervention in the study group was significantly higher than that in the control group (P<0.05). A remarkably lower incidence of adverse cardiovascular events after intervention was observed in the study group in comparison to the control group (P<0.05). Patients in the study group had significantly higher ESCA, GQOLI-74 and MMAS-8 scores and lower HAD scores than those in the control group (all P<0.001).
Conclusion: Early multi-dimensional cardiac rehabilitation nursing for patients undergoing PCI can significantly improve the patients’ adherence to medication and quality of life. It can also reduce the incidence of adverse cardiovascular events. It has remarkable nursing efficacy, and is worthy of more widespread promotion and clinical application.
Keywords: early multi-dimensional cardiac rehabilitation nursing, PCI, cardiovascular disease
1 INTRODUCTION
Coronary heart disease (CHD) is a broad term encompassing several closely related syndromes caused by myocardial ischemia (an imbalance between cardiac blood supply and myocardial oxygen and nutritional demands). Because cardiac myocytes generate energy almost exclusively through mitochondrial oxidative phosphorylation, cardiac function is strictly dependent upon the continuous flow of oxygenated blood through the coronary arteries. In more than 90% of cases, CHD is a consequence of reduced coronary blood flow secondary to obstructive atherosclerotic vascular disease. Thus, unless otherwise specified, CHD usually is synonymous with coronary artery disease. Another term that is synonymous with CHD is ischemic heart disease. The various clinical features of CHD are consequences of coronary atherosclerosis that has been gradually progressing for decades. The manifestations of CHD are a direct consequence of the insufficient blood supply to the heart. The clinical presentation may include one or more of the following cardiac syndromes: (1) Angina pectoris: This term literally means “chest pain”. It occurs when the degree of ischemia is sufficient to induce pain but insufficient to cause myocyte death. Angina can be stable (occurring predictably at certain levels of exertion), or can be caused by vessel spasm (Prinzmetal’s angina), or can be unstable (occurring with progressively less exertion or even at rest). Fixed obstructions that occlude less than 70% of a coronary vessel lumen typically are asymptomatic, even with exertion. In comparison, lesions that occlude more than 70% of a vessel lumen result in the so-called “critical stenosis” and generally cause symptoms in the setting of increased demand. With critical stenosis, certain levels of exertion predictably cause chest pain, and the patient is said to have stable angina. A fixed stenosis that occludes 90% or more of a vascular lumen can lead to inadequate coronary blood low with symptoms even at rest, one of the forms of unstable angina. (2) Myocardial infarction (MI). This occurs when the severity or duration of ischemia is sufficient to cause cardiomyocyte death. And (3) Sudden cardiac death (SCD). This can occur as a consequence of tissue damage from MI, but most commonly results from a lethal arrhythmia without myocyte necrosis.
The term acute coronary syndrome is applied to any of the 3 catastrophic manifestations of CHD (unstable angina, MI and SCD).
Depending on the specific manifestation of CHD, as well as its severity, treatment can either be pharmacological or non-pharmacological. The former includes such drugs as calcium channel blockers, beta-blockers, nitrates, thrombolytics, etc. The latter includes percutaneous coronary intervention (PCI) and coronary artery bypass grafting. Except for PCI, other treatment methods are beyond the scope of this article and will not be discussed any further.
PCI is a widely used cardiac catheterization technique in clinical practice that is capable of restoring patency in stenosed coronary arteries to improve myocardial perfusion[1-3]. It involves passing a fine guidewire across a coronary stenosis under radiographic control and using it to position a balloon, which is then inflated to dilate the stenosis. This can be combined with deployment of a coronary stent, which is a piece of metallic ‘scaffolding’ that can be impregnated with drugs with antiproliferative properties and that helps to maximize and maintain dilatation of a stenosed vessel. Treatment with PCI is less traumatic and often provides excellent symptom control with rapid postoperative recovery. The main acute complications of PCI are occlusion of the target vessel or a side branch by thrombus, and consequent myocardial damage. The main long-term complication of PCI is restenosis, which may occur in up to a quarter of cases. The efficacy of PCI may be compromised by patients’ negative emotions and psychological pressure at the time of surgery[4,5]. Despite the significant clinical efficacy of PCI in the treatment of CHD, clinical studies have revealed that the procedure is marred by an array of issues in the postoperative period. These include such issues as a high incidence of cardiovascular adverse events and poor patient adherence to medication. Therefore, effective nursing interventions are very important in patients undergoing PCI[6-8]. With the improvement of living standards, patients have more stringent requirements for perioperative nursing when undergoing PCI. Conventional nursing fails to meet the clinical needs of patients due to its multiple shortcomings. As a new type of nursing model, early multi-dimensional cardiac rehabilitation nursing yields a significant nursing effect in patients that have undergone PCI[9-14]. To evaluate the application value of early multi-dimensional cardiac rehabilitation nursing in PCI and its effect on adverse events and patients’ adherence to medication, this study selected a total of 90 patients that underwent PCI in our hospital between 2019 and 2020 as the study subjects. Our findings are presented herein under.
2 MATERIALS AND METHODS
2.1 General Information
A total of 90 patients that underwent PCI in our hospital from January 2019 to January 2020 were selected as the study subjects. The patients were divided into two groups according to the order of admission, the control group and the study group, with 45 patients in each group. There were 25 male and 20 female patients in the control group. The average age of the patients was 56.29±3.1 years and the average BMI was 25.06±1.58kg/m2. 30 patients were assigned to class I and 15 were assigned to class II of the Killip classification. 6 patients had disease in 1 arterial branch, 17 in 2 arterial branches and 22 in 3 arterial branches. 28 of the patients were smokers, and 26 drank alcohol. There were 26 male and 19 female patients in the study group. The average age of the patients was 56.23±3.6 years and the average BMI was 24.89±1.64kg/m2. 33 patients were assigned to class I and 12 were assigned to class II of the Killip classification. 7 patients had disease in 1 arterial branch, 15 in 2 arterial branches and 23 in 3 arterial branches. 30 of the patients were smokers, and 29 drank alcohol.
2.2 Inclusion Criteria
The inclusion criteria in the present study were as follows: (1) Patients who underwent PCI for the first time and the surgery was successful; and (2) Patients that were aged at least 18 years of age.
2.3 Exclusion Criteria
The exclusion criteria in the present study were as follows: (1) Patients with mental disorders; (2) Patients who were required to undergo a second PCI; and (3) Patients with a left ventricular ejection fraction <30%.
It must be stated that all patients enrolled into this study as well as their family members were informed about the study, and all of them signed the Informed Consent form. The study protocol was reviewed and approved by the medical ethics committee of Cangzhou Central Hospital (approval number 20190190).
2.4 Methods
Patients in the control group received conventional nursing. This included basic nursing, diet nursing, health education and medication guidance.
Patients in the study group received conventional nursing (same as that described for the control group) and early multi-dimensional cardiac rehabilitation nursing. The specific procedures included: (1) A regular schedule was formulated for the patients. They were instructed to perform exercises of large muscle groups and joints on a regular basis. The precautions and treatment goals of PCI were also explained to the patients in detail. (2) The actual situation of the patients was recorded in detail to evaluate their physical condition and formulate feasible nursing protocols. (3) Clinical psychological evaluation of patients was conducted to formulate targeted psychological nursing protocols according to the patient's psychological status. Psychological counseling and guidance were provided for patients with severe anxiety or depression to alleviate these negative emotions. (4) After surgery, patients were assisted in slow walking by nursing staff and instructed to cultivate good living habits. Factors that interfere with cardiac rehabilitation were also explained in detail to the patients. (5) The patients were instructed to follow the doctor's advice after surgery. The patients' cardiac rehabilitation intervention files were established for further review, with patients' privacy protected. A WeChat official account was established to provide knowledge related to the patients' disease, diet regimens, perioperative precautions, exercise rehabilitation programs and medication guidance through videos and articles. (6) Active communication with patients was conducted after PCI. The patients’ health status was comprehensively evaluated based on their actual situations. Patient's that had certain bad habits were advised to correct said bad habits in order to improve their self-nursing abilities. (7) Negative emotions such as anxiety and depression harbored by patients were closely observed during communication. Psychological comfort was provided to subjects with intense emotional changes. A clean and tidy treatment environment was provided for the patients and clear instructions concerning medication were given. The clinical response was closely monitored to avoid adverse events. And (8) Dietary intervention was conducted according to every patient’s individual needs by maintaining nutritional balance, less spicy and cold food and provision of sufficient amounts of protein and vitamins.
2.5 Observational Indicators
(1) Nursing satisfaction: The "Patient Clinical Satisfaction Questionnaire" prepared by our department was used to assess the nursing satisfaction of patients. The highest possible score on this questionnaire is 100 points. The higher the score, the higher the satisfaction.
(2) Adverse cardiovascular events: The incidence of adverse cardiovascular events in patients in the two groups before and after the intervention was compared. Adverse cardiovascular events include heart failure, arrhythmia, MI and angina pectoris.
(3) Self-care agency scale (ESCA) score: This was used to evaluate the self-care ability of patients after intervention. The scale includes such items as self-concept, self-responsibility, self-care skills, and level of health knowledge. Each item has a total score of 4 points. The higher the score, the higher the patient's self-care ability.
(4) Generic quality of life inventory-74 (GQOLI-74) score: This was used to assess the patients’ quality of life after intervention. The scale includes such items as mental function, physical function, social function and material life status. The highest possible score is 100. The higher the score, the better the patient’s quality of life.
(5) Morisky medication adherence scale 9 (MMAS-8) score: This was used to assess the patients’ adherence to medication before and after intervention. The highest possible score is 8. The higher the score, the higher the adherence to medication.
(7) Hospital anxiety and depression scale (HAD) score: This was used to assess the patient's emotional state before and after intervention. The highest possible score is 42. The higher the score, the greater the severity of the patient’s anxiety and depression.
2.6 Statistical Analysis
The data obtained in this study was processed using SPSS20.0. GraphPad Prism 7 (GraphPad Software, San Diego, USA) was used to plot the graphs. The research data included counting data and measurement data. Counting data was processed using the X2 test, while the measurement data was analyzed using the t and normality tests. P<0.05 indicates statistical significance.
3 RESULTS
3.1 General Information
There were no significant differences in the age, gender, BMI, Killip classification, number of diseased arterial branches, type of medical insurance, number of smokers and number of alcohol drinkers between patients in the two groups (P>0.05). See Table 1 for details.
Table 1. Comparison of General Information between the Two Groups of Patients [n (%)]
Indicators |
Study Group (n=45) |
Control Group (n=45) |
X2 or t |
P |
Gender |
|
|
0.045 |
0.832 |
Male |
26 (57.78) |
25 (55.56) |
|
|
Female |
19 (42.22) |
20 (44.44) |
|
|
Age (years) |
|
|
0.085 |
0.933 |
|
56.23±3.6 |
56.29±3.1 |
|
|
BMI (kg/m2) |
|
|
0.501 |
0.618 |
|
24.89±1.64 |
25.06±1.58 |
|
|
Killip Classification |
|
|
0.476 |
0.490 |
Ⅰ |
33 (73.33) |
30 (66.67) |
|
|
Ⅱ |
12 (26.67) |
15 (33.33) |
|
|
Number of diseased branches |
|
|
|
|
1 |
7 (15.56) |
6 (13.33) |
0.089 |
0.764 |
2 |
15 (33.33) |
17 (37.78) |
0.194 |
0.660 |
3 |
23 (51.11) |
22 (48.89) |
0.044 |
0.833 |
Medical insurance form |
|
|
|
|
Medical insurance |
17 (37.78) |
16 (35.56) |
0.048 |
0.827 |
New rural cooperative medical insurance |
20 (44.44) |
19 (42.22) |
0.045 |
0.832 |
Self-sponsored |
8 (17.78) |
10 (22.22) |
0.278 |
0.598 |
Smoking |
|
|
0.194 |
0.660 |
Yes |
30 (66.67) |
28 (62.22) |
|
|
No |
15 (33.33) |
17 (37.78) |
|
|
Drinking |
|
|
0.421 |
0.517 |
Yes |
29 (64.44) |
26 (57.78) |
|
|
No |
16 (35.56) |
19 (42.22) |
|
|
3.2 Nursing Satisfaction
Patients in the study group were more satisfied with nursing in comparison to those in the control group (P<0.05). See Table 2 for details.
Table 2. Comparison of Nursing Satisfaction between the Two Groups of Patients [n (%)]
Group |
n |
Satisfied |
Moderately Satisfied |
Dissatisfied |
Total Satisfaction |
Study group |
45 |
68.89% (31/45) |
24.44% (11/45) |
8.89% (3/45) |
93.33% (42/45) |
Control group |
45 |
48.89% (22/45) |
22.22% (10/45) |
28.89% (13/45) |
71.11% (32/45) |
x2 |
|
|
|
|
7.601 |
P |
|
|
|
|
<0.05 |
3.3 Incidence of Adverse Cardiovascular Events
The incidence of adverse cardiovascular events after intervention was lower among patients in the study group compared to those in the control group (P<0.05). See Table 3 for details.
Table 3. Comparison of the Incidence of Adverse Cardiovascular Events between the Two Groups of Patients [n(%)]
Group |
n |
Heart Failure |
Arrhythmia |
MI |
Angina Pectoris |
Total Incidence |
Study group |
45 |
2.22% (1/45) |
0.00% (0/45) |
2.22% (1/45) |
4.44% (2/45) |
8.89% (4/45) |
Control group |
45 |
6.67% (3/45) |
8.89% (4/45) |
6.67% (3/45) |
8.89% (4/45) |
31.11% (14/45) |
x2 |
|
|
|
|
|
6.944 |
P |
|
|
|
|
|
<0.05 |
3.4 ESCA Score
Patients in the study group obtained significantly higher ESCA scores than their counterparts in the control group after intervention (P<0.05). See Table 4 for details.
Table 4. Comparison of ESCA Scores between the Two Groups of Patients (mean±SD, points)
Group |
n |
Self-concept |
Self-responsibility |
Self-care Skills |
Level of Health Knowledge |
Study group |
45 |
2.71±0.82 |
2.32±0.61 |
2.73±0.45 |
3.13±0.31 |
Control group |
45 |
1.33±0.52 |
1.15±0.32 |
1.21±0.12 |
1.52±0.63 |
t |
|
9.534 |
11.394 |
21.894 |
15.382 |
P |
|
<0.001 |
<0.001 |
<0.001 |
<0.001 |
3.5 GQOLI-74 Score
Patients in the study group obtained significantly higher GQOLI-74 scores than their counterparts in the control group after intervention (P<0.05). See Table 5 for details.
Table 5. Comparison of GQOLI-74 Scores between the Two Groups of Patients (mean±SD, points)
Group |
n |
Mental Function |
Physical Function |
Social Function |
State of Material Life |
Study group |
45 |
81.44±5.72 |
84.28±5.78 |
84.25±6.53 |
85.63±6.98 |
Control group |
45 |
62.11±4.68 |
61.22±4.65 |
64.88±4.25 |
64.25±5.71 |
t |
|
17.545 |
20.823 |
16.677 |
15.904 |
P |
|
<0.001 |
<0.001 |
<0.001 |
<0.001 |
3.6 MMAS-8 Score
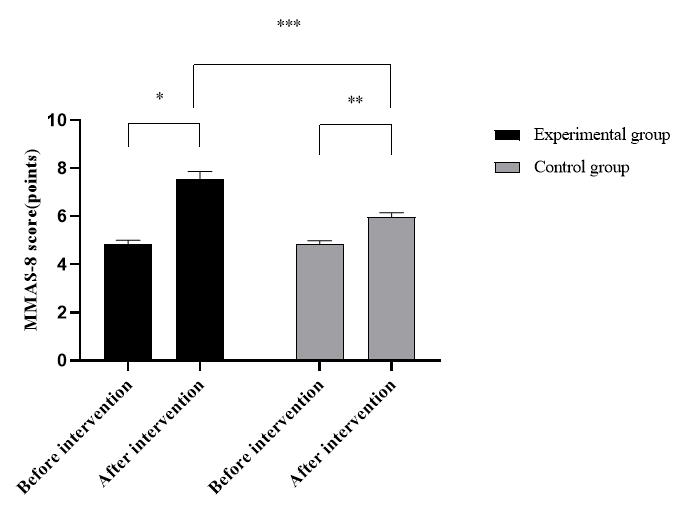
Patients in the study group obtained significantly higher MMAS-8 scores than their counterparts in the control group after intervention (P<0.05). See Figure 1 for details.
|
Figure 1. Comparison of MMAS-8 scores between the two groups of patients (mean±SD). The abscissa indicates before and after the intervention, and the ordinate indicates MMAS-8 score, points; The MMAS-8 scores of patients in the experimental group before and after intervention were (4.85±0.15) points and (7.56±0.31) points respectively; The MMAS-8 scores of the control group before and after intervention were (4.84±0.15) points and (5.98±0.17) points respectively; * indicates that there is a significant difference in the MMAS-8 scores of the experimental group before and after nursing intervention (t=52.788, P<0.001); ** indicates that there is a significant difference in the MMAS-8 scores of the control group patients before and after the nursing intervention (t=33.731, P<0.001); *** indicates that there is a significant difference in the MMAS-8 scores of the two groups of patients after nursing intervention (t=29.978, P<0.001).
3.7 HAD Score
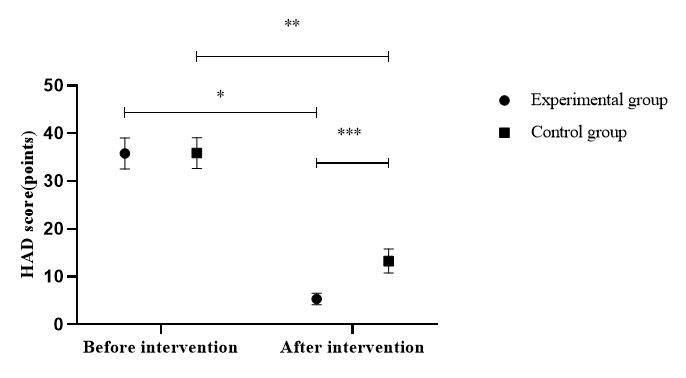
Patients in the study group obtained lower HAD scores than their counterparts in the control group after intervention (P<0.05). See Figure 2 for details.
|
Figure 2. Comparison of HAD scores between the two groups of patients (mean±SD). The abscissa indicates before and after the intervention, and the ordinate indicates HAD score, points; The HAD scores of the patients in the experimental group before and after intervention were (35.81±3.25) points and (5.36±1.21) points respectively; The HAD scores of the control group before and after intervention were (35.88±3.22) points and (13.29±2.53) points respectively; * indicates that there is a significant difference in the HAD scores of the experimental group before and after intervention (t=58.901, P<0.001); ** indicates that there is a significant difference in the HAD scores of the control group before and after intervention (t=37.005, P<0.001); *** indicates that there is a significant difference in the HAD scores of the two groups of patients after intervention (t=18.968, P<0.001).
4 DISCUSSION
PCI is the main treatment for severe CHD. It can relieve coronary vascular obstruction and reduce patient mortality. Despite its remarkable efficacy, it cannot eliminate the risk factors related to CHD[15-17]. It has been found that most patients still face a risk of coronary vascular re-stenosis after PCI. This underscores the significance of effective nursing interventions to improve prognosis in patients[18,19]. Conventional nursing is currently adopted in most hospitals. However, inadequate communication and interaction with patients as occurs with conventional nursing fails to meet the patients' psychological demands. This may easily trigger negative emotions such as irritability and anxiety in both patients and their families. This is anything but helpful in the establishment of a harmonious nurse-patient relationship, and may even affect the hospital’s reputation in extreme cases. Early multi-dimensional cardiac rehabilitation nursing has been recognized as an emerging nursing model. It is a comprehensive, systematic, standardized, and patient-centered nursing model that provides an excellent nursing environment and humanistic care to patients, alleviates negative emotions, creates a harmonious patient-nurse relationship, and enhances the quality of nursing[20,21].
In this study, the HAD score of patients in the study group after intervention was significantly lower than that of those in the control group (P<0.05). This indicates that compared with conventional nursing, early multi-dimensional cardiac rehabilitation nursing can partially or totally eliminate patients' negative emotions. It has been pointed out that early multi-dimensional cardiac rehabilitation nursing is a continuous and multi-dimensional nursing model that explains the importance of cardiac rehabilitation nursing to patients through health education, rehabilitation training, and psychological care[22]. In this study, the incidence of adverse cardiovascular events in the study group after intervention was significantly lower than that in the control group (P<0.05). This suggests that early multi-dimensional cardiac rehabilitation nursing is a safe nursing model. Early multi-dimensional cardiac nursing can effectively enhance the patient’s cognition of their own disease, improve their self-care ability, correct their bad habits, and help establish a positive attitude toward the disease by active communication and interaction. This is cardinal in boosting recovery in the postoperative period[23,24]. While nursing patients, the medical team provides precautions that patients undergoing PCI must take before surgery, implements health education and provides knowledge related to the patients’ disease. This is done to alleviate negative emotions, and to build up patient confidence toward treatment. After hospital discharge, patients were made to follow or subscribe to WeChat official accounts, which were then used to follow up the patients' actual condition and provide nursing guidance. These WeChat official accounts were also used to share information regarding nursing and disease. This was done to raise the patient's awareness towards their disease, improve self-care ability, reduce the incidence of complications and improve the patient's quality of life. In this study, the ESCA and MMAS-8 scores of patients in the study group after intervention were significantly higher than those of patients in the control group (P<0.05). This indicates that early multi-dimensional cardiac rehabilitation nursing can reinforce patients” adherence to medication and self-care ability. The results of this study also showed that the total nursing satisfaction of patients in the study group after intervention was significantly higher than that of those in the control group (P<0.05). This finding is consistent with the results of Gadelhak et al.[25], which pointed out that "the total satisfaction of nursing in the study group (95.12%) was significantly higher than that observed in the control group (78.15%) (P<0.05)", suggesting that early multi-dimensional cardiac rehabilitation nursing holds the promise of a better nursing quality.
Despite the strengths of our study, we wish to state that it is marred a few limitations. These include a small sample size and short observational duration, which are required to be improved in the future studies to obtain more reliable data.
5 CONCLUSION
Early multi-dimensional cardiac rehabilitation nursing for patients undergoing PCI can significantly improve the patients’ adherence to medication and quality of life. It can also reduce the incidence of adverse cardiovascular events. It has remarkable nursing efficacy, and is worthy of more widespread promotion and clinical application.
Acknowledgements
Not applicable.
Conflicts of Interest
The authors declared no conflict of interest.
Author Contribution
All authors contributed to the manuscript and approved the final version.
Abbreviation List
CHD, Coronary heart disease
ESCA, Self-care agency scale
GQOLI-74, Generic quality of life inventory-74
HAD, Hospital anxiety and depression scale
MI, Myocardial infarction
MMAS-8, Morisky medication adherence scale 9
PCI, Percutaneous coronary intervention
SCD, Sudden cardiac death
References
[1] Schwaab B, Zeymer U, Jannowitz C et al. Improvement of low-density lipoprotein cholesterol target achievement rates through cardiac rehabilitation for patients after ST elevation myocardial infarction or non-ST elevation myocardial infarction in Germany: Results of the patient care registry. Eur J Prev Cardiol, 2019; 26: 249-258. DOI:10.1177/2047487318817082
[2] Chandrasekaran AM, Kinra S, Ajay VS et al. Effectiveness and cost-effectiveness of a Yoga-based Cardiac Rehabilitation (Yoga-CaRe) program following acute myocardial infarction: Study rationale and design of a multi-center randomized controlled trial. Int J Cardiol, 2019; 280: 14-18. DOI:10.1016/j.ijcard.2019.01.012
[3] Taylor RS, Sadler S, Dalal HM et al. The cost effectiveness of REACH-HF and home-based cardiac rehabilitation compared with the usual medical care for heart failure with reduced ejection fraction: A decision model-based analysis. Eur J Prev Cardiol, 2019; 26: 1252-1261. DOI:10.1177/2047487319833507
[4] Kamiya K, Yamamoto T, Tsuchihashi-Makaya M et al. Nationwide survey of multidisciplinary care and cardiac rehabilitation for patients with heart failure in Japan-An analysis of the AMED-CHF study. Circ J, 2019; 83: 1546-1552. DOI:10.1253/circj.CJ-19-0241
[5] Mendell J, Bates J, Banner-Lukaris D et al. What do patients talk about? A qualitative analysis of online chat sessions with health care specialists during a “virtual” cardiac rehabilitation program. Telemed E-Health, 2019; 25: 71-78. DOI:10.1089/tmj.2017.0206
[6] Sherwood MW, Vora AN. Challenges in aortic stenosis: Review of antiplatelet/anticoagulant therapy management with transcatheter aortic valve replacement (TAVR): TAVR with recent PCI, TAVR in the patient with atrial fibrillation, and TAVR thrombosis management. Curr Cardiol Rep, 2018; 20: 1-6. DOI:10.1007/s11886-018-1073-9
[7] Schüpke S, Hein-Rothweiler R, Mayer K et al. Revacept, a novel inhibitor of platelet adhesion, in patients undergoing elective PCI-Design and rationale of the randomized ISAR-PLASTER trial. Thromb Haemostasis, 2019; 119: 1539-1545. DOI:10.1055/s-0039-1692423
[8] Kosugi S, Suzuki N, Kumagai N et al. Dominance of angular momentum exchange in the PCI recapture of photoelectrons revealed by high resolution Auger electron measurements of Kr. J Phys B-At Mol Opt, 2019; 52: 245002.
[9] Ge Z, Baber U, Claessen BE et al. The prevalence, predictors and outcomes of guideline‐directed medical therapy in patients with acute myocardial infarction undergoing PCI, an analysis from the PROMETHEUS registry. Catheter Cardio Inte, 2019; 93: E112-E119. DOI:10.1002/ccd.27860
[10] Bhatt DL, Steg PG, Mehta SR et al. Ticagrelor in patients with diabetes and stable coronary artery disease with a history of previous percutaneous coronary intervention (THEMIS-PCI): A phase 3, placebo-controlled, randomised trial. Lancet, 2019; 394: 1169-1180. DOI:10.1016/S0140-6736(19)31887-2
[11] Ibrahim H, Kaltenbach LA, Hess CN et al. Glycoprotein IIb/IIIa inhibitor use in patients with acute myocardial infarction undergoing PCI: Insights from the TRANSLATE ACS study. Catheter Cardio Inte, 2019; 93: E204-E210. DOI:10.1002/ccd.27816
[12] Korjian S, Daaboul Y, Laliberté F et al. Cost implications of anticoagulation strategies after percutaneous coronary intervention among patients with atrial fibrillation (a PIONEER-AF PCI analysis). Am J Cardiol, 2019; 123: 355-360. DOI:10.1016/j.amjcard.2018.10.033
[13] Liosis S, Hochadel M, Darius H et al. Effect of renal insufficiency and diabetes mellitus on in-hospital mortality after acute coronary syndromes treated with primary PCI. Results from the ALKK PCI Registry. Int J Cardiol, 2019; 292: 43-49. DOI:10.1016/j.ijcard.2019.04.071
[14] Finn MT, Redfors B, Karmpaliotis D et al. Adverse events in patients with high platelet reactivity following successful chronic total occlusion PCI: The assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Am Heart J, 2019; 211: 68-76. DOI:10.1016/j.ahj.2019.02.002
[15] Pandey P, Sharma LN. Image processing techniques applied to satellite data for extracting lineaments using PCI geomatica and their morphotectonic interpretation in the parts of northwestern Himalayan frontal thrust. J Indian Soc Remote, 2019; 47: 809-820. DOI:10.1007/s12524-019-00962-2
[16] Hotta M, Minamimoto R, Gohda Y et al. Impact of a modified peritoneal cancer index using FDG-PET/CT (PET-PCI) in predicting tumor grade and progression-free survival in patients with pseudomyxoma peritonei. Eur Radiol, 2019; 29: 5709-5716. DOI:10.1007/s00330-019-06102-1
[17] Witlox WJA, Ramaekers BLT, Groen HJM et al. Factors determining the effect of prophylactic cranial irradiation (PCI) in patients with stage-III nonsmall cell lung cancer: exploratory subgroup analyses of the NVALT-11/DLCRG-02 phase-III study. Acta Oncol, 2019; 58: 1528-1531. DOI:10.1080/0284186X.2019.1629016
[18] Vranckx P, Valgimigli M, Eckardt L et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): A randomised, open-label, phase 3b trial. Lancet, 2019; 394: 1335-1343. DOI:10.1016/S0140-6736(19)31872-0
[19] Bagai J, Hess E, Penny WF et al. Outcomes of Transradial PCI compared to Transfemoral PCI in veterans with anemia: Insight from the VA Clinical Assessment, Reporting and Tracking (CART) program. Cardiovasc Revasc Med, 2019; 20: 990-996. DOI:10.1016/j.carrev.2019.01.014
[20] Kim YH, Her AY, Jeong MH et al. A comparison between statin with ACE inhibitor or ARB therapy in STEMI patients who underwent successful PCI with drug-eluting stents. Atherosclerosis, 2019; 289: 109-117. DOI:10.1016/j.atherosclerosis.2019.08.018
[21] Chieffo A, Burzotta F, Pappalardo F et al. Clinical expert consensus document on the use of percutaneous left ventricular assist support devices during complex high-risk indicated PCI: Italian society of interventional cardiology working group endorsed by Spanish and Portuguese interventional cardiology societies. Int J Cardiol, 2019; 293: 84-90. DOI:10.1016/j.ijcard.2019.05.065
[22] Shariff M, Kumar UA. Ample evidence for statins preloading before PCI on periprocedural myocardial infarction among stable angina pectoris patients undergoing percutaneous coronary intervention. Cardiovasc Revasc Med, 2019; 20: 533-534. DOI:10.1016/j.carrev.2019.03.017
[23] Tolika K. On the analysis of the temporal precipitation distribution over Greece using the Precipitation Concentration Index (PCI): Annual, seasonal, monthly analysis and association with the atmospheric circulation. Theor Appl Climatol, 2019; 137: 2303-2319. DOI:10.1007/s00704-018-2736-6
[24] Guedeney P, Claessen BE, Mehran R et al. Small-vessel PCI outcomes in men, women, and minorities following platinum chromium everolimus-eluting stents: Insights from the pooled PLATINUM diversity and PROMUS element plus post-approval studies. Catheter Cardiovasc Interv, 2019; 94: 82-90. DOI:10.1002/ccd.28071
[25] Gadelhak B, Tawfik AM, Saleh GA et al. Extended abdominopelvic MRI versus CT at the time of adnexal mass characterization for assessing radiologic peritoneal cancer index (PCI) prior to cytoreductive surgery. Abdom Radiol, 2019; 44: 2254-2261. DOI:10.1007/s00261-019-01939-y
Copyright © 2022 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.





 Copyright ©
Copyright ©