Application Effect of Mobile Nurse Stations Combined with Refined Management in Patients with Postpartum Depression
Jingjing Ma1, Junxia Ma1*
1Cangzhou Central Hospital, Hebei Province, China
*Correspondence to: Junxia Ma, Nurse-in-Charge, Cangzhou Central Hospital, No.16 West Xinhua Road, Cangzhou City 061000, Hebei Province, China; Email: 1003516691@qq.com
Abstract
Objective: To provide insight into the application effect of mobile nurse stations combined with refined management in the nursing of patients with postpartum depression (PPD).
Methods: 120 patients with PPD admitted to our hospital in the past two years were selected as the study subjects. The patients were randomly segregated into group A and group B. Group A was given mobile nurse stations with refined management, while group B was administered with refined management alone. A comparative analysis of the psychological status of the 2 groups of patients was performed using the Addison PPD scale (EPDS). Nursing-related indicators, nursing deficit rate, quality of life (QOL), and nursing satisfaction between the 2 groups of patients were also compared.
Results: The psychological status of patients in group A was significantly better than that of patients in group B after 6 months of nursing intervention (P<0.001). The PPD rate in group A was significantly lower than that in group B after 20 days and 6 months (P<0.05). The patients' language communication and nursing operation time were significantly longer for group A than for group B (P<0.001). In contrast, the number of trips to and from the nurse's stations and the number of times patients rang their bedside bells per day in group A was significantly lower than that of patients in group B (P<0.001). Group A exhibited a significantly lower nursing error rate than group B (P<0.05). In addition, the QOL domains scores of patients in group A were significantly higher than those of patients in group B (P<0.001). The nursing satisfaction of patients in group A patients was significantly higher than that of patients in group B (P<0.05).
Conclusion: Taken together, these findings suggest that the combination of mobile nurse stations and the refined management model positively impacts the mental state of women with PPD, reduces the possibility of nursing errors, improves the comprehensive nursing effect and optimizes the maternal QOL. Therefore, further research is needed to investigate the effectiveness of this model, and to understand the intricacies of its implementation in clinical practice.
Keywords: mobile nurse station, EPDS, PPD, QOL, mental state
1 INTRODUCTION
The period after delivery of a child is known as the postpartum period[1]. During this time, women are susceptible to the impact of various complications such as the stress of labor and an array of other psychiatric disorders, a constellation of symptoms that is commonly known as postpartum depression (PPD)[2]. PPD often occurs one or two weeks after delivery. Women suffering from PPD usually show adverse psychological conditions such as depression, psychomotor agitation or retardation[3]. In severe cases, the patients may develop pessimism and world-weariness. Their physical function may be affected to varying degrees, causing a significant negative impact on their physical and mental health[1-3]. Conventional postpartum care pays more attention to protecting the maternal and infant physical health, with very little attention paid to the puerpera’s psychological health. To relieve symptoms of PPD and improve women's psychological health by determining their unfulfilled psychological needs, a nursing mode with refined management and improved service is imperative. Refined management refers to a concept of excellent postpartum nursing that is centered on the puerpera with the aim to provide a better postpartum nursing experience[4-7]. The mobile nurse station has been preliminarily applied in clinical practice, which provides on the palm work platform attached to the hospital information management system. Through a personal digital assistant (PDA), nurses can easily search and share medical information to achieve better mobile nursing service, which theoretically has a high value for refined management. In light of the above stated literature, the present study aimed to explore the combined effect of mobile nursing stations with refined management application in the management of PPD.
2 MATERIALS AND METHODS
2.1 Study Design
A total of 120 patients with PPD admitted to our hospital in the past two years were included in this study. The patients were randomly divided into group A and group B. The study is comprised of two phases. The first phase recruited patients with PPD, whereas the second phase examined the efficacy of refined management provided with nursing stations. The baseline data such as age, gestational age (in weeks), and gestational times between the two groups of patients were analyzed (P>0.05).
2.2 Sampling Strategy
Patients with PPD were randomly selected after meeting the eligibility criteria set for the current study. The patients were divided into two groups, which were statistically compared for psychological status. The study scheme has been approved by the hospital's Ethical Committee led by the medical superintendent, clinicians, the head nurse, ethicists, secretaries, and medical specialists among others.
2.3 Inclusion Criteria
The inclusion criteria in the present study were as follows:
(1) Patients aged at least 18 years of age.
(2) Patients who had adequate proficiency in the Chinese language.
(3) Patients who gave birth to a healthy infant at our hospital.
(4) Patients who were identified as having PDD by the Addison PPD scale (EPDS) core.
2.4 Exclusion Criteria
Patients were excluded from the study if:
(1) They had diseases in other organ diseases.
(2) They were diagnosed with a mental disorder or had difficulties communicating.
(3) They had a history of depression.
2.5 Implementation Steps
Patients in group A were treated with mobile nurse stations with refined management mode, while those in group B were only subjected to refined management. The specific implementation steps of the two nursing modes were as follows.
2.5.1 Mobile Nursing Station
(1) The nursing staff were trained to access and efficiently use PDA. This enabled them to accurately master the relevant functions and application methods used, changed their traditional handwritten nursing records, and enabled them to use PDA throughout the study.
(2) This study was equipped with a total of 10 PDAs. Considering the fact that women with PPD were more likely to have a rather depressed mood at night, the charging time of the devices was set at 8am.
(3) The nurses would search the relevant records of the patient using PDA before implementation of any nursing interventions. Meanwhile, nurses also monitored real-time relevant information of the puerpera through PDA, generated daily nursing record sheets to facilitate the review and summary, and to improve the quality of nursing.
(4) In the course of nursing, the staff were able to identify the puerpera’s needs with the help of PDA, and took corresponding measures where needed.
(5) Nursing staff communicated with the puerpera in a timely manner to understand the latter’s emotional changes, and then went on to record the details on PDA. This was done to keep an accurate record of the puerpera’s psychological state. The mental health of the nursing staff was regularly assessed and appropriate interventions were carried out when needed[8-11].
2.5.2 Refined Management
(1) Refinement of nursing problems: Nursing staff held meetings with the patients. Firstly, the everyday problems of the patients were summarized so as to understand their psychological status. The probable causes of depression were sought according to physical symptoms and daily performance, with the aim of providing the corresponding interventions. Secondly, an analysis of the problems in current postpartum nursing was carried out. For instance, considering the completion of treatment task as the nursing goal, ignoring the psychological state of puerpera, insufficient knowledge regarding PDD, etc. The nursing staff proposed a corresponding optimization plan to accomplish resource sharing and improve their problem-solving efficiency.
(2) Refinement of nursing management and establishment of a strict system with shared responsibility: To ensure nursing efficacy and consistency, the nursing staff took a shift every 3 months to accurately comprehend the psychological dynamic changes and data of physical indicators. During the handover after shift change, the nursing staff summarized the problems during the shift and arranged them into a table (group A with PDA, group B with paper). The head nurse graded the nursing staff during the handover to evaluate the nursing efficacy.
(3) Refinement of nursing quality: Nursing staff got a thorough understanding of the puerpera they were responsible for and paid more attention to the quality of nursing. They gave full play to their subjective initiative according to the personal situation of puerpera, closely observed the physical data and psychological status of puerpera, and strictly prevented the possibility of various accidents. In addition, the nursing staff provided a good rest space for the puerpera, and strived to improve the quality of nursing through multiple interventions.
(4) Refinement of psychological education: Lectures were held on pregnancy and delivery, and the participation of puerpera and the relatives was ensured. At least three lectures were arranged, and the relatives were recommended to accompany the puerpera in rotation to promote awareness of pregnancy and childbirth among puerpera and their families. The lectures included knowledge on maternal and child health, childbirth and common postpartum diseases among other topics. These lectures were provided with a view to informing family members about the current situation of the puerpera, enhance care and reduce the pressure associated with pregnancy and childbirth. In addition, the nursing staff encouraged the puerpera to fully express themselves, and helped them find ways to get rid of any negative emotions, enhance their outlook on life, improve their psychological state, and reduce the degree of depression[12-15].
2.6 Outcome Measures
The criteria for examining the curative effect in the current study were maternal psychological status, EPDS score, nursing-related indicators, nursing defect rate, quality of life (QOL), and nursing satisfaction.
(1) Psychological status: The self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were used as the basis for assessing the psychological status. A score above 49 indicated an adverse psychological status. The scores were taken 20 days and 6 months after the comprehensive nursing intervention.
(2) EPDS score: A score of 13 or above was consistent with PPD. The scores were evaluated 20 days and 6 months after the implementation of comprehensive nursing intervention.
(3) Nursing-related indicators: These included the time of language communication between nurses and puerpera, nursing operation time, the number of visits to and from the nurse's station, and the number of times patients rang their bedside bell per day.
(4) Nursing error rate: This included the doctor’s orders and reports verification error, missed dispensing, and prescription of the wrong medicine. The total incidence was then calculated.
(5) QOL score: The self-rating scale was used to assess the emotions, role function, physical function, and social function. The score ranged from 0 to 100. The lower the score, the poorer the QOL.
(6) Nursing satisfaction: This was evaluated from a range of 0-5 stars. 5 stars indicated that the patient was extremely satisfied, 3-4 stars indicated that the patient was satisfied, and 2 stars or less indicated that the patient was dissatisfied with nursing.
2.7 Statistical Analysis
SPSS 20.0 was used for data processing, and GraphPad Prism 7 (GraphPad Software, San Diego, USA) was used to illustrate the data figures. The data included in the study comprised counting data and measurement data using the Chi-square test and student t-test for statistical analysis. P<0.05 was considered statistically significant. The number of samples was calculated using G*Power software.
3 RESULTS
3.1 Psychological Status
The SAS and SDS scores of patients in group A were significantly lower than those of patients in group B after 6 months, with improved psychological status (P<0.001). See Table 1 for details.
Table 1. Comparison of Psychological Status of the Puerpera at Different Intervals (mean±SD)
Group |
20 Days |
6 Months |
||
SAS |
SDS |
SAS |
SDS |
|
Group A |
53.50±4.52 |
54.41±4.23 |
21.56±4.21 |
25.21±3.59 |
Group B |
53.59±4.50 |
55.10±4.05 |
36.56±4.01 |
38.56±3.45 |
t |
0.109 |
0.913 |
19.984 |
20.769 |
P |
0.913 |
0.363 |
0.000 |
0.000 |
3.2 EPDS Scores
Patients in group A had a lower PPD rate than those in group B after 20 days and 6 months of nursing interventions (P<0.05). See Table 2 for details.
Table 2. Comparison of EPDS of Puerpera at Different Intervals [n(%)]
Group |
20 Days |
PPD Rate |
6 Months |
PPD Rate |
||
<13 |
≥13 |
<13 |
≥13 |
|||
Group A |
14 |
46 |
46 (76.7) |
59 |
1 |
1 (1.7) |
Group B |
5 |
55 |
55 (91.7) |
36 |
24 |
24 (40.0) |
X2 |
|
|
5.065 |
|
|
26.728 |
P |
|
|
0.024 |
|
|
0.000 |
3.3 Nursing-related Indicators
Patients in group A were found to have longer communication and nursing operation times than those in group B (P<0.001). The number of trips to and from the nurse's station and the number of times patients rang their bedside bells per day in group A was significantly lower than that in group B (P<0.001). See Table 3 for details.
Table 3. Comparison of Nursing-related Indicators of Puerpera (mean±SD)
Group |
Language Communication Time (min) |
Nursing Operation Time (min) |
Number of Trips to and from the Nurse's Station |
Number of Times Patients Rang Their Bells |
Group A |
15.3±0.1 |
12.1±2.2 |
20.0±2.5 |
7.5±0.5 |
Group B |
6.8±0.2 |
8.5±1.0 |
33.5±2.1 |
12.5±1.1 |
t |
294.449 |
11.539 |
32.028 |
32.053 |
P |
0.000 |
0.000 |
0.000 |
0.000 |
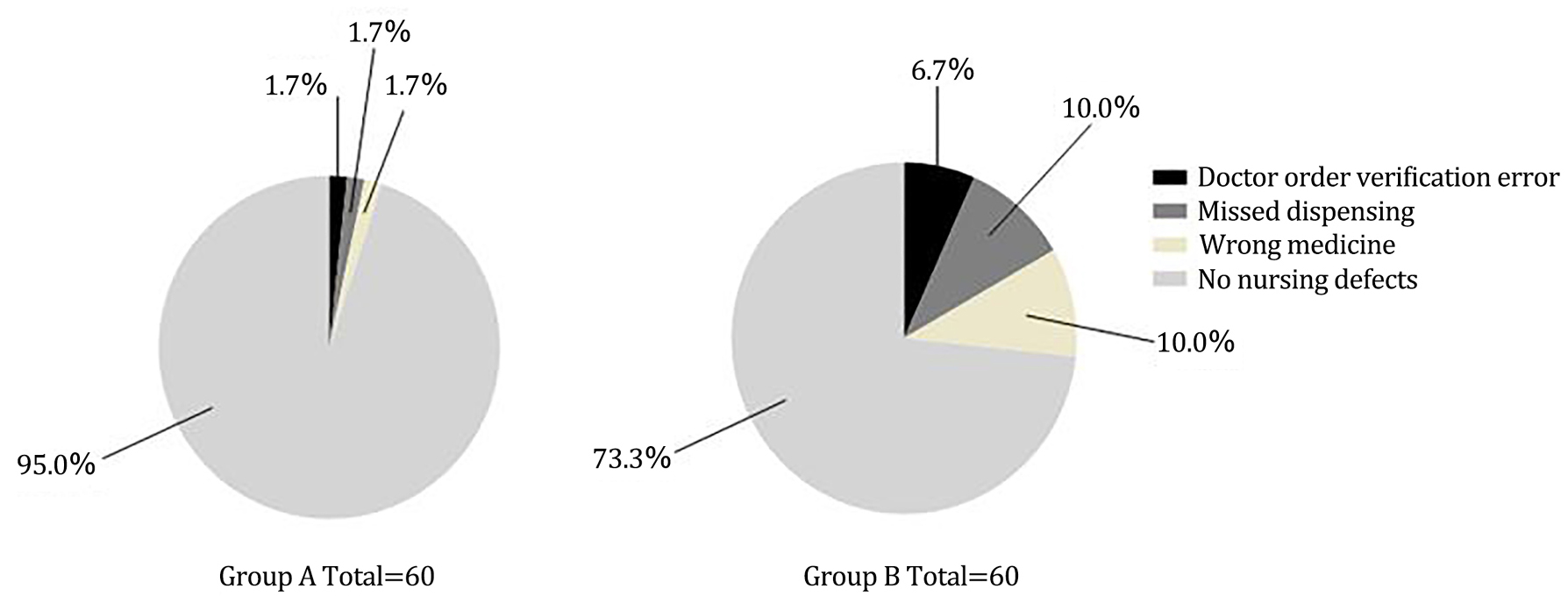
3.4 Nursing Defect Rate
The nursing defect rate of group A was significantly lower than that of group B (P<0.05). See Figure 1 for details.
|
Figure 1. Comparison of nursing defect rate of purpera. NB: The legend on the right shows what the respective colors mean. There was 1 case of doctor order verification error, 1 case of missed dispensing, 1 case of prescription of the wrong medicine, and 57 cases without any errors in group A. There were 4 cases of doctor order verification error, 6 cases of missed dispensing, 6 cases of prescription of the wrong medicine and 44 cases without any errors in group B.
3.5 QOL Scores
Patients in group A had significantly higher QOL scores than their counterparts in group B (P<0.001). See Figure 2A for details.
3.6 Nursing Satisfaction
The findings revealed that patients in group A were more satisfied with nursing in comparison to their counterparts in group B (P<0.05), and the difference was statistically significant. See Figure 2B for details.
|
Figure 2. Comparison of QOL scores between the two groups of patients (mean±SD) (A) and comparison of nursing satisfaction of puerperal (B). A: The horizontal axis shows emotional function, role function, physical function, and social function from left to right. The four scores of group A were (78.59±1.10), (80.52±1.21), (60.59±1.02), and (75.52±1.20), respectively. The four scores of group B were (54.56±1.15), (60.21±2.56), (54.15±1.10), and (63.21±1.32) respectively. * indicates that P<0.001; B: The horizontal axis shows the number of extremely satisfied cases, satisfied cases, unsatisfied cases and totally satisfied cases from left to right. There were 42 cases, 16 cases, 2 cases, and 58 cases in group A, and 18 cases, 32 cases, 10 cases and 50 cases in group B respectively. * indicates that P<0.001, and # indicates that P<0.05.
4 DISCUSSION
The findings of the comparative analysis of the current study revealed that the use of mobile nurse stations combined with the refined management model has a positive effect on improving the mental state of women with PPD. Puerpera are usually in a fragile state after childbirth and are easily disturbed by external and internal factors. PPD has a global prevalence, and profoundly impacts maternal physical and mental health. Traditional postpartum nursing predominantly focuses on the functional status of mother and infant, while paying little or no attention to the mother’s psychological health. However, refined management has the advantage of tailoring medications to specific cases. The overall nursing quality is improved, which plays a role in reducing the degree of PPD and improving puerpera's physical and mental health[16-19]. With continuous innovation and advances in the fields of science and technology, extensive research is needed to evaluate the effectiveness of this approach and understand the intricacies behind the implementation of mobile nurse stations. This kind of nursing method can improve accuracy, reduce the possibility of nursing defects, and have a high coordination effect for refined nursing.
In this study, patients in group A showed significantly improved psychological status after 6 months of comprehensive nursing intervention in comparison to those in group B. A lower PPD rate was observed in group A, which proves that mobile nurse stations could optimize the intervention efficiency of nursing staff as they take care of patients with PPD. Refined management can improve the puerpera's understanding of PPD and their knowledge of pregnancy and delivery. The nursing staff who applied refined management paid more attention to communication with the puerpera, so the psychological status of the puerpera showed significant improvement, while the PPD rate showed a decreasing trend.
The language communication time and nursing operation time of nursing staff in group A were significantly longer than in group B. The number of trips to and from the nurse's station and the number of times patients rang their bedside bells per day in group A was significantly lower than that in group B. The nursing error rate in group A was significantly lower than that in group B, suggesting that refined management had a prominent nursing effect by providing specific solutions for specific problems. The nursing staff improved their ability to communicate with the puerpera. By efficiently apprehending the advantages of PDA, the nursing staff reduced the possibility of making errors in group A and responded more favorably to the puerpera's needs, making it more acceptable for the puerpera. The nursing satisfaction of patients in group A was significantly higher than that of those in group B. Similar findings were obtained in a previous study, which stated that nursing care and problem-solving training can confidently be used in the primary care setting for women with symptoms of PPD[20,21].
Under the influence of the above factors, the puerpera in group A experienced less pressure from their family and received more meticulous care. As such, their QOL scores were significantly higher than those in group B. This proved that the comprehensive nursing intervention model played a positive role in coping with PDD[22,23]. Previous studies applied a high-quality nursing model with refined management to puerpera with PDD in the study group. The comprehensive QOL score of the puerpera in this group was measured to be (80.56±5.12), significantly higher than that of those puerpera in the control group (which used conventional nursing). This confirms the positive effect of refined management on the rehabilitation of puerpera with PDD[24]. The results mentioned above strengthen the study's main objective and are consistent with the results obtained in this article.
Our study team experienced some challenges in designing the study's methodological concept. As we already know, this was a control study, and a control study requires a large sample size. Our small sample size was the most prominent limiting factor. Another significant limiting factor was that nursing staff had insufficient knowledge of PPD.
5 CONCLUSION
In conclusion, the application of mobile nurse stations with refined management can effectively improve the psychological status of puerpera, reduce the degree of PPD and improve the quality of comprehensive nursing. It is an approach that merits further promotion in clinical practice.
Acknowledgments
The authors are thankful to all the participants for providing us with samples. We are also thankful to the hospital management for helping us during the study period.
Conflicts of Interest
The authors declared no conflict of interest.
Author Contribution
All authors contributed to the manuscript and approved the final version.
Abbreviation List
EPDS, Addison PPD scale
PDA, Personal digital assistant
PDD, Postpartum depression
QOL, Quality of life
SAS, Self-rating anxiety scale
SDS, Self-rating depression scale
References
[1] Logsdon MC, Vogt K, Davis DW et al. Screening for postpartum depression by hospital-based perinatal nurses. MCN Am J Matern Child Nurs, 2018; 43: 324-329. DOI: 10.1097/NMC.0000000000000470
[2] Guintivano J, Putnam KT, Sullivan PF et al. The international postpartum depression: Action towards causes and treatment (PACT) consortium. Int Rev Psychiatry, 2019; 31: 229-236. DOI: 10.1080/09540261.2018.1551191
[3] Fathi F, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M. Maternal self-efficacy, postpartum depression, and their relationship with functional status in Iranian mothers. Women Health, 2018; 58: 188-203. DOI: 10.1080/03630242.2017.1292340
[4] Baumel A, Tinkelman A, Mathur N et al. Digital peer-support platform (7 Cups) as an adjunct treatment for women with postpartum depression: Feasibility, acceptability, and preliminary efficacy study. JMIR Mhealth Uhealth, 2018; 6: e38. DOI: 10.2196/mhealth.9482
[5] Weissman MM. Postpartum depression and its long-term impact on children: many new questions. JAMA Psychiatry, 2018; 75: 227-228. DOI: 10.1001/jamapsychiatry.2017.4265
[6] Pérez F, Catalán A, Morales A et al. Assessment of postpartum depression in a group of Chilean parents. J Men Health, 2018; 14: 56-64. DOI: 10.22374/1875-6859.14.2.7
[7] Watanabe K, Ishii K, Ishida H et al. Antenatal parenting class aiming to enhance empathy between partners for prevention of postpartum depression: A trial at a hospital to assess attendantsʼ empathy level and mental health status and to verify their evaluation of the session. Jap J of Health Hum Ecol, 2019; 85: 80-89. DOI: 10.3861/kenko.85.2_80
[8] Amini S, Jafarirad S, Amani R. Postpartum depression and vitamin D: A systematic review. Crit Rev Food Sci Nutr, 2019; 59: 1514-1520. DOI: 10.1080/10408398.2017.1423276
[9] Mundorf C, Shankar A, Moran T et al. Reducing the risk of postpartum depression in a low-income community through a community health worker intervention. Matern Child Health J, 2018; 22: 520-528. DOI: 10.1007/s10995-017-2419-4
[10] Kim Y, Dee V. Sociodemographic and obstetric factors related to symptoms of postpartum depression in hispanic women in rural California. J Obstet Gynecol Neonatal Nurs, 2018; 47: 23-31. DOI: 10.1016/j.jogn.2017.11.012
[11] O'Hara MW, Engeldinger J. Treatment of postpartum depression: Recommendations for the clinician. Clin Obstet Gynecol, 2018; 61: 604-614. DOI: 10.1097/GRF.0000000000000353
[12] Tobin CL, Di Napoli P, Beck CT. Refugee and immigrant women's experience of postpartum depression: A meta-synthesis. J Transcult Nurs, 2018; 29: 84-100. DOI: 10.1177/1043659616686167
[13] Shulman B, Dueck R, Ryan D et al. Feasibility of a mindfulness-based cognitive therapy group intervention as an adjunctive treatment for postpartum depression and anxiety. J Affect Disord, 2018; 235: 61-67. DOI: 10.1016/j.jad.2017.12.065
[14] Waldrop J, Ledford A, Perry LC et al. Developing a postpartum depression screening and referral procedure in pediatric primary care. J Pediatr Health Care, 2018; 32: e67-e73. DOI: 10.1016/j.pedhc.2017.11.002
[15] Ma H. The preventive and therapeutic effects of prenatal nursing intervention on postpartum depression [in Chinese]. China Foreign Med Treat, 2019; 38: 130-132. DOI: 10.16662/j.cnki.1674-0742.2019.32.130
[16] Maxwell D, Robinson SR, Rogers K. "I keep it to myself": A qualitative meta-interpretive synthesis of experiences of postpartum depression among marginalised women. Health Soc Care Comm, 2019; 27: e23-e36. DOI: 10.1111/hsc.12645
[17] Ilska M, Banaś E, Gregor K et al. Vaginal delivery or caesarean section-Severity of early symptoms of postpartum depression and assessment of pain in Polish women in the early puerperium. Midwifer, 2020; 87: 102731. DOI: 10.1016/j.midw.2020.102731
[18] Akram B, Ahmed MA, Maqsood F et al. postpartum depression and suicidal ideation in new mothers with hearing loss: Perceived social support as a moderator, a multicentre study. J Pak Med Assoc, 2020; 70: 213-218. DOI: 10.5455/JPMA.11537
[19] Johar H, Hoffmann J, Günther J et al. Evaluation of antenatal risk factors for postpartum depression: A secondary cohort analysis of the cluster-randomised GeliS trial. BMC Med, 2020; 18: 227. DOI: 10.1186/s12916-020-01679-7
[20] Simonds W. Watching the clock: Keeping time during pregnancy, birth, and postpartum experiences. Soc Sci Med, 2002; 55: 559-70. DOI: 10.1016/s0277-9536(01)00196-4
[21] Meltzer-Brody S, Maegbaek ML, Medland SE et al. Obstetrical, pregnancy and socio-economic predictors for new-onset severe postpartum psychiatric disorders in primiparous women. Psychol Med, 2017; 47: 1427-1441. DOI: 10.1017/S0033291716003020
[22] Burke L. The impact of maternal depression on familial relationships. Int Rev Psychiatr, 2003; 15: 243-55. DOI: 10.1080/0954026031000136866
[23] Tezel A, Gözüm S. Comparison of effects of nursing care to problem solving training on levels of depressive symptoms in post-partum women. Patient Educ Couns, 2006; 63: 64-73. DOI: 10.1016/j.pec.2005.08.011
[24] Anna Sue. How does the quality of nursing affect women with postpartum depression. Health Soc Care Comm, 2020.
Copyright © 2022 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.






 Copyright ©
Copyright ©