Effects of the Humanized Nursing Model in Obstetric Nursing Based on the Use and Gratification Theory
Lizhen Luo1, Jinjin Liu1*
1The Obstetrics Department, Shiyan Maternal and Child Health Hospital, Shiyan, China
*Corresponding to: Jinjin Liu, Bachelor, the Obstetrics Department, Shiyan Maternal and Child Health Hospital, No. 9 Kaixuan Avenue, Zhangwan District, Shiyan City 442000, China; Email: 644615055@qq.com
Abstract
Objective: To explore the application effect of the humanized nursing model in obstetric nursing based on the use and gratification theory.
Methods: A total of 148 parturients who were hospitalized in the Obstetrics Department of our hospital from January 2018 to January 2020 were selected as the study subjects. The parturients were then divided into 2 groups, the study group and the control group, based on the order of maternal admission in a ratio of 1:1. Routine obstetric nursing was implemented for patients in the control group. For patients in the study group, an analysis of their needs for humanized care based on the use and gratification theory was performed and a humanized nursing model was constructed. The Edinburgh postnatal depression scale (EPDS), general self-efficacy scale (GSES-C32), and Berlin social support scale (SSS) were used to assess the depression, self-efficacy and social support of patients in the two groups before and after nursing. The pregnancy outcomes and nursing satisfaction of patients in the two groups were also compared.
Results: There was no significant difference in the EPDS scores between patients from the two groups before nursing (P>0.05). There was a significant reduction in the EPDS scores of patients from both groups after nursing, with greater reductions seen in patients from the study group than their counterparts in the control group (P<0.05). There was no significant difference in the total efficiency expectation (EE-16), outcome expectation (OE-16) and GSES-C32 scores between patients from the two groups before nursing (P>0.05). After treatment, there was a significant increase in these parameters in patients from both groups, with the increase being more pronounced in the study group than the control group (P<0.05). There was no significant difference in the utilization of subjective support, objective support, social support and total scores between the two groups before nursing (P>0.05). After nursing, there was a significant increase in the utilization of subjective support, objective support, social support and total scores in patients from both groups. The increase was more pronounced in the study group than in the control group (P<0.05). The rates of cesarean deliveries, neonatal asphyxia and postpartum hemorrhage of patients in the study group were lower than those of patients in the control group (P<0.05). The rate of nursing satisfaction in the study group was 97.30%, significantly higher than that of 86.49% seen in the control group (P<0.05).
Conclusion: The humanized nursing model in obstetric nursing based on the use and gratification theory is a reliable strategy in obstetric nursing. It can reduce postpartum anxiety and depression, enhance self-efficacy and social support, improve pregnancy outcomes and increase nursing satisfaction.
Keywords: use and gratification theory, humanized, nursing model, obstetrics, parturients, effect
1 INTRODUCTION
Puerperium (defined as the time from delivery of the placenta to return of the uterus to its normal pre-pregnancy size, usually 6 weeks) and childbirth are inevitable links in maternal life. During labor, women often experience severe pain. This is especially true for primiparas (women who are giving birth for the first time). Due to their lack of awareness of childbirth or difficulty in adapting to the mother's role, they usually experience a series of negative emotions such as tension, anxiety and depression[1]. In addition, fetal movement and weight-bearing cause increases in blood pressure and heart rate, and may also induce sleep disorders. This in turn causes patients to be poorly compliant to treatment. Negative emotions may also lead to postpartum uterine contractions, increased rates of cesarean delivery and risk of childbirth[2,3]. Current routine obstetric care in health centers ignores maternal needs and emotions, thus hindering pregnancy outcomes[4]. Following the rapid development of the Internet that has occurred in recent years, the use and gratification theory has gradually been applied in nursing and medical fields as a new method of solving problems. The use and gratification theory was proposed by the American scholar Katz. It is based on the needs and desires of individuals to use the media in a social environment and obtain satisfaction from these needs[5]. It emphasizes on the individual’s initiative to change the individual’s active behavioral pattern[6]. With the transformation of modern nursing modes, people are no longer satisfied with routine basic nursing. Humanized nursing has become a new trend in the development of modern nursing modes. It can improve nurses' awareness of active service and provide patients with the best quality nursing services[7,8]. Therefore, it is imperative to clinically explore more precise, optimized and humanized nursing interventions.
In the past, there was a paucity of studies reporting on the effect of the humanized nursing model based on the use and gratification theory in obstetric nursing. Therefore, this study attempts to compare the efficacy of routine obstetric nursing and the humanized nursing model based on use and gratification theory in obstetric nursing.
2 MATERIALS AND METHODS
2.1 Participants
A total of 148 patients admitted to the obstetrics department of our hospital from January 2018 to January 2020 were included in this study. A random number table was established using SPSS23.0 software, and the participants were randomly assigned into two groups. Before enrollment, the study obtained the informed consent of the patients, and the study protocol was approved by the Hospital Ethics Committee (grant number: ES-XDE20180103), and all procedures were in compliance with the ethical guidelines outlined in the Declaration of Helsinki.
Inclusion criteria: (1) Primipara with singleton pregnancies who received examination at our hospital on a regular basis; (2) Patients with complete clinical data; and (3) Patients who provided informed consent.
Exclusion criteria: (1) Patients with vital organ dysfunction e.g. heart, liver, kidney, lung, etc.; (2) Patients with severe pregnancy and labor complications; (3) Patients with coagulation disorders and indications for cesarean delivery; and (4) Patients with lallopathy, cognitive disorders or mental disorders.
Termination criteria: (1) Subjects that experienced serious adverse reactions or complications during the study, or whose condition worsened; (2) Subjects who quit the study voluntarily; and (3) Subjects who underwent other treatment methods during the study period. Upon termination, a case would not be included in the statistics, and other subjects would be included.
According to the order of maternal admission, patients were divided into a study group and a control group, with 74 cases in each group. Patients in the control group were aged between 20 and 36 years old, with an average of (28.37±5.24) years. The gestational week was between 36 and 40 weeks, with an average of (39.21±2.53) weeks. The body mass index (BMI) was between 23.12 and 28.25kg/m2, with an average BMI of (25.46±2.38)kg/m2. Educational background: 21 cases of junior middle school or below, 25 cases of senior high school level, 28 cases of junior college, college or above. Patients in study group were aged between 21 and 38 years old, with an average of (28.80±5.30) years. The gestational age was between 37 and 41 weeks, with an average of (39.14±2.46) weeks. The BMI was between 23.09 and 28.27kg/m2, with an average of (25.50±2.37)kg/m2. Educational background: 19 cases of junior middle school or below, 26 cases of senior high school, 29 cases of junior college, college or above. The baseline data of patients in the two groups was balanced.
2.2 Methods
Patients in the control group received routine obstetric care. This included monitoring of maternal vital signs before delivery to understand the general condition of the expectant mothers. The patients were also taught how to take deep breaths and maintain a comfortable position during delivery, and were also provided with guidance on neonatal care after delivery or discharge. Out-of-hospital rehabilitation manuals were distributed, and the new mothers were reminded to come for their reviews on time.
Patients in the study group received a humanized nursing model based on the use and gratification theory. The patients received a questionnaire on humanized nursing needs that included prevention of prenatal and postpartum depression, postpartum uterine and wound recovery, neonatal care, breastfeeding, postpartum nutrition and postpartum exercise. According to the results of the survey and maternal needs, a humanized nursing model was established. (1) Mental nursing: Since the women are primiparas, they may bear a relatively heavy psychological burden and easily experience anxiety and depression before and after childbirth. Therefore, nursing staff should pay due attention to the parturients’ mental health and enhance communication with them, so as to learn about their worries and help them to build a good mindset. Nursing staff should also communicate with the parturients’ family members to obtain more knowledge about the parturients’ condition. Family members may also take part in the mental nursing for parturients. (2) Health education: Due to the lack of knowledge about childbirth and labor pain in primiparas, it is easy for them to develop negative emotions. Doctors and nurses should improve the patients’ knowledge and understanding of the process of childbirth, and strengthen nursing interventions through health education applicable to primiparas. (3) Physiological care: The nursing staff should ensure that the soon to be mother maintains a positive and enthusiastic attitude before entering the delivery room. She must be informed about the advantages and disadvantages vaginal delivery and cesarean section. She must also be taught how to mitigate the pain associated with labor. There should be adequate family and social support for primiparas. In addition, nursing staff should help mothers familiarize themselves with the layout and environment of the delivery room. Mothers should be encouraged to comply with follow-up treatment, and their sense of security should be heightened. After delivery, nursing staff should monitor the mother and newborn in real time and promptly respond to anything that goes wrong. Nursing staff should provide individualized nursing care to each mother. It is not a good idea to impart complex and diverse knowledge to the new mothers, as this tends to affect their understanding and mastery of childbirth and motherhood. Relevant content should be compiled in a manual to help mothers and their families understand what they need to understand. (4) Environmental care: Maternal recovery is closely related to the external environment. An appropriate environment that is sterile and well ventilated must be ensured. (5) Diet and exercise care: After the mother is discharged from the hospital, she can take part in diet and exercise counseling provided by the nursing staff through platforms such as WeChat. This allows the new mother to voice out her feelings, experiences and opinions. Diet and exercise plans should be formulated for the new mothers to help facilitate the recovery process. Excessive exercise in the immediate postpartum period should be strongly discouraged, as it can lead to postpartum injuries. (6) Nursing staff should visit mothers once a month to learn about their family support, assess their physical and mental state, and guide their recovery.
2.3 Observation Indicators and Efficacy Determination
(1) Edinburgh postnatal depression scale (EPDS) scores: The EPDS[9] was used to evaluate the mental state of parturients in the two groups before and after nursing. The scale consists of 10 items namely fear, anxiety, mood, insomnia, enjoyment, sadness, self-blame, crying, self-harm and reaction ability. A score of 1,2 or 3 is given if the patient occasionally, often or always experiences a given feeling respectively. The highest possible total score is 30. Higher scores indicate greater maternal depression.
(2) General self-efficacy scale (GSES-C32)[9] score: The GSES-C32 was used to evaluate the self-efficacy for parturients in the two groups before and after nursing. It included two parallel scales, the efficiency expectation (EE-16) and the outcome expectation (OE-16). These scales each contain 16 items, and each item is divided into 10 grades. Higher scores indicate higher maternal self-efficacy.
(3) Social support scale (SSS) score: SSS was used to compare social support for parturients in the two groups before and after nursing. It comprises subjective support, objective support and utilization of social support, each containing 10 items. Items are scored on a scale of 1 to 5, where 1 indicates that the respondent considers the statement to be completely false, and 5 indicates they consider the statement completely true. Higher scores indicate more social support.
(4) Pregnancy outcomes: Pregnancy outcomes mainly included the rate of cesarean deliveries, neonatal asphyxia and 2-hour postpartum hemorrhage volume.
(5) Nursing satisfaction: A satisfaction scale prepared by our hospital was used to evaluate the satisfaction of the parturients with nursing. The evaluation mainly covered communication skills, service attitude, nursing skills, health education and humanistic care, with total score of 100. A total score of greater than 80 was considered to be satisfactory, that of 60-80 was considered to be relatively satisfactory, and that below 60 was considered to be unsatisfactory. Higher scores indicated better satisfaction. The total satisfaction rate was worked out using the formula: (Satisfactory + relatively satisfactory) / total number of cases ×100%.
2.4 Statistical Analysis
The study data was analyzed and processed using the SPSS 18.0 software. Measurement data was tested by Shapiro-Wilk line for normal distribution. Normally distributed measurement data was expressed as mean standard deviation. The independent samples t test was used for homogeneity of variance, and the independent samples t test was used for unequal variance. The paired samples t test was used for comparison before and after treatment within a given group. The enumeration data was described as a percentage (%) and processed with the Chi-square test. Statistical significance was assumed at P<0.05.
3 RESULTS
3.1 Comparison of EPDS Scores
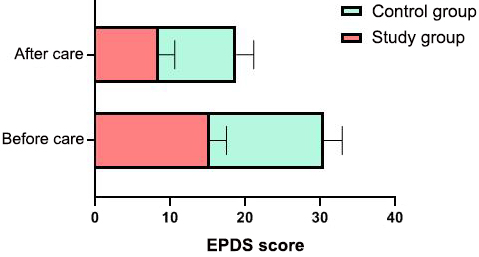
There was no significant difference in the EPDS scores between patients from the two groups before nursing (P>0.05). There was a significant reduction in the EPDS scores of patients from both groups after nursing, with greater reductions seen in patients from the study group than their counterparts in the control group (P<0.05). See Figure 1 for details.
|
Figure 1. Comparison of EPDS scores of the two groups of parturients before and after nursing.
3.2 Comparison of GSES-C32 Scores
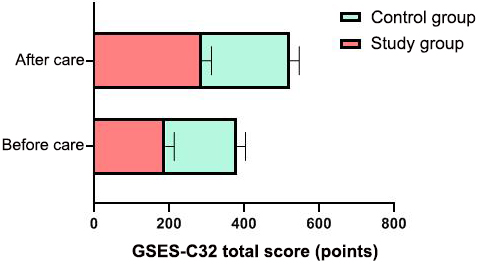
There was no significant difference in the total EE-16, OE-16 and GSES-C32 scores between patients from the two groups before nursing (P>0.05). After treatment, there was a significant increase in these parameters in patients from both groups, with the increase being more pronounced in the study group than the control group (P<0.05). See Table 1 and Figure 2 for details.
Table 1. Comparison of Self-efficacy Scores between the Two Groups Before and After Nursing (Score, mean±SD)
Group |
EE-16 |
OE-16 |
GSES-C32 |
|||
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
|
Study group (n=74) |
96.33±17.68 |
126.34±20.37a |
94.09±16.35 |
127.40±21.03a |
189.34±23.56 |
287.13±25.30a |
Control group (n=74) |
96.37±17.57 |
113.86±18.71 a |
94.21±16.43 |
114.54±18.42 a |
190.12±23.48 |
235.09±24.11 a |
t |
0.014 |
3.881 |
0.044 |
3.957 |
0.202 |
12.810 |
P |
0.989 |
<0.001 |
0.964 |
<0.001 |
0.840 |
<0.001 |
Notes: aP<0.05 vs. the situation before nursing in the same group.
|
Figure 2. Comparison of total GSES-32 scores of the two groups before and after nursing.
3.3 Comparison of SSS Scores
There was no significant difference in the utilization of subjective support, objective support, social support and total scores between the two groups before nursing (P>0.05). After nursing, there was a significant increase in the utilization of subjective support, objective support, social support and total scores in patients from both groups. The increase was more pronounced in the study group than in the control group (P<0.05). See Table 3 for details.
Table 2. Comparison of SSS Scores between the Two Groups Before and After Nursing
Group |
Subjective Support |
Objective Support |
Utilization of Social Support |
Total Score |
||||
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
|
Study group (n=74) |
17.16±2.56 |
26.48±3.05a |
9.52±1.47 |
13.34±1.75a |
5.37±2.03 |
9.85±2.63a |
31.16±5.31 |
49.15±5.76a |
Control group (n=74) |
17.20±2.58 |
21.56±2.79a |
9.48±1.46 |
11.28±1.67a |
5.40±2.06 |
7.21±2.26a |
31.22±5.29 |
41.44±5.43a |
t |
0.095 |
10.240 |
0.166 |
7.326 |
0.089 |
6.549 |
0.069 |
8.379 |
P |
0.870 |
<0.001 |
0.970 |
<0.001 |
0.985 |
<0.001 |
0.975 |
<0.001 |
Notes: aP<0.05 vs. the situation before nursing in the same group.
3.4 Comparison of Pregnancy Outcomes
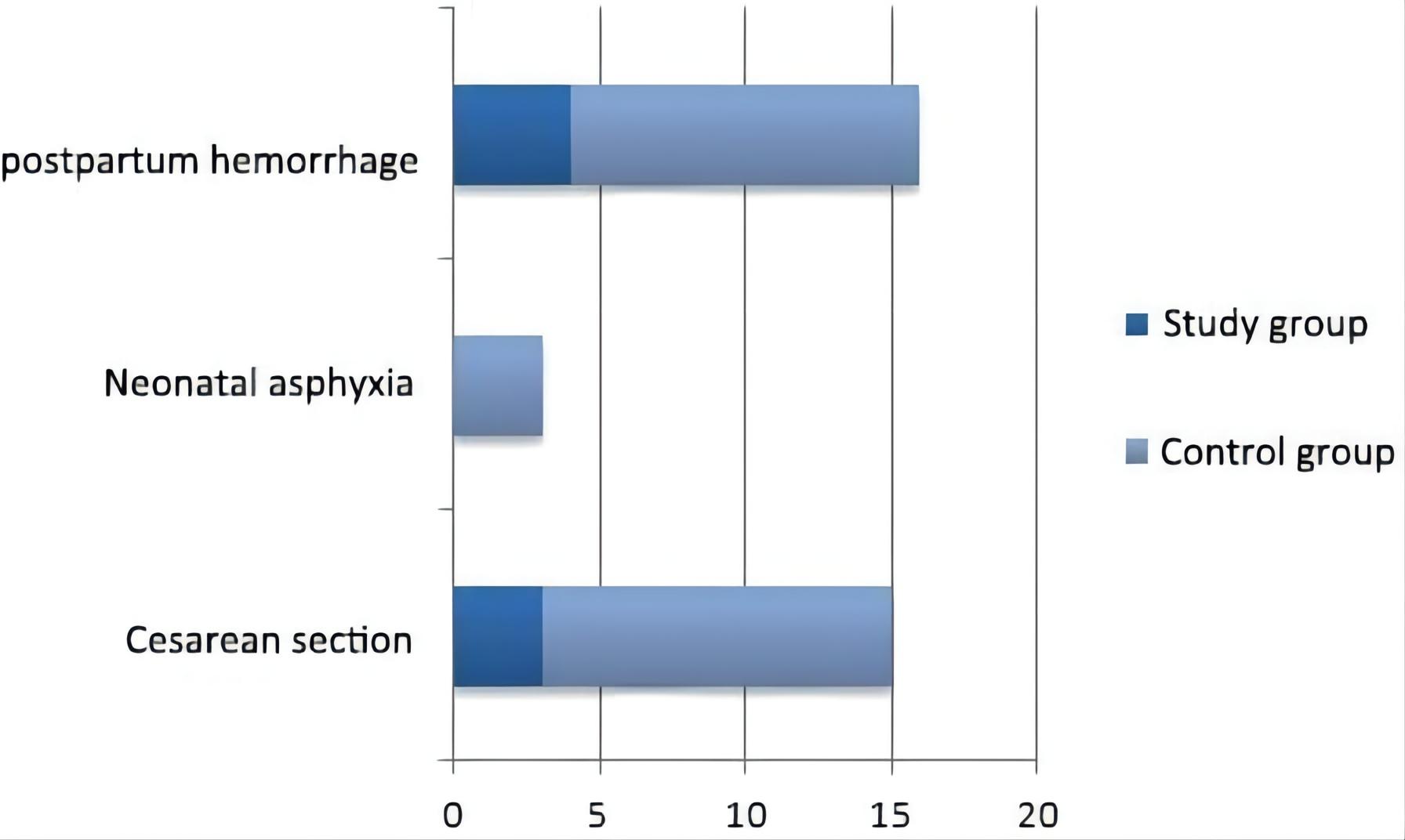
The rates of cesarean deliveries, neonatal asphyxia and postpartum hemorrhage of patients in the study group were lower than those of patients in the control group (P<0.05). See Table 3 and Figure 3 for details.
Table 3. Comparison of Pregnancy Outcomes between the Two Groups (n, %)
Group |
Cesarean Deliveries |
Neonatal Asphyxia |
Postpartum Hemorrhage |
Study group (n=74) |
3 (4.05) |
0 (0.00) |
4 (5.41) |
Control group (n=74) |
12 (16.22) |
3 (4.05) |
13 (17.57) |
χ2 |
6.009 |
5.895 |
5.383 |
P |
0.014 |
0.015 |
0.020 |
|
Figure 3. Comparison of pregnancy outcomes between the two groups.
3.5 Comparison of Nursing Satisfaction between the Two Groups
The rate of nursing satisfaction in the study group was 97.30%, significantly higher than that of 86.49% seen in the control group (P<0.05). See Table 4 for details.
Table 4. Comparison of Nursing Satisfaction between the Two Groups (n, %)
Group |
Satisfactory |
Relatively Satisfactory |
Unsatisfactory |
Total Satisfaction Rate |
Study group (n=74) |
58 (77.42) |
14 (19.35) |
2 (2.70) |
72 (97.30) |
Control group (n=74) |
30 (38.71) |
34 (45.16) |
10 (13.51) |
64 (86.49) |
χ2 |
|
|
|
5.804 |
P |
|
|
|
0.016 |
4 DISCUSSION
Most mothers experience changes in their psychological status and social roles during pregnancy and childbirth. This is especially true for primiparas, who have to bear the pressures of family life, physical discomfort, hormone secretion and social influence[6]. Relevant studies have shown that the incidence of postpartum depression in foreign countries is 3.5%-33%, while the incidence of postpartum depression in China is 4.5%-20%[10,11]. Some maternal stress factors in the prenatal period may affect normal delivery, prolong the delivery process and affect pregnancy outcomes[12]. Routine obstetric care solely focuses on the distribution and promotion of oral and rehabilitation manuals. However, it lacks humanistic care. Therefore, it is imperative that effective nursing intervention and health education is implemented for pregnant women[13,14].
The results of the study showed that the EPDS score of patients in the study group after nursing was lower than that of those in the control group. This indicates that the application of the humanized nursing model based on the use and gratification theory can effectively reduce postpartum depression. It emphasizes the leading role and subjective initiative of the client in the service process, and formulates corresponding nursing measures according to the needs of the client. Humanized nursing models should be established with the needs of the expectant mothers in mind[15]. This is consistent with the findings of Li[16] and Medeiros et al[17]. This study investigated maternal needs for humane care, women’s perception of childbirth, usage of knowledge and information, and how women use the media. A nursing program was then developed on this basis. In the plan, health education is disseminated according to the needs and interests of the patients. This nursing model helps mothers to actively learn about postpartum recovery and reduce postpartum depression.
Primiparas often face various problems during the puerperal period due to lack of experience, knowledge and limited ability to take care of themselves. This is anything but conducive to the growth and development of neonates. It also affects postpartum recovery and reduces self-efficacy[18,19]. The study results showed that after nursing, the total EE-16, OE-16 and GSES-C32 scores of patients in both groups increased significantly. However, the increase was more pronounced in the study group than the control group. This suggests that the combination of the humanized nursing model and the use and gratification theory can effectively improve maternal self-efficacy. The humanized nursing model and the use and gratification theory are based on the needs of the expectant mothers. Through enhanced communication with expectant mothers, nursing staff can get a better understanding of their psychological state of and help them establish a positive attitude towards pregnancy and childbirth. Through strengthened nursing interventions, nursing staff can improve patients’ knowledge, explain the advantages and disadvantages of labor, and explain the differences between vaginal and cesarian delivery. They can also educate primiparas on how to mitigate the pain associated with labor and enhance family and social support[20]. Nursing staff should help mothers familiarize themselves with the layout and environment of the delivery room to prevent them from rejecting follow-up treatment and to enhance their sense of security[21].
The results also showed that the subjective support, objective support, social support utilization rate and total score of patients in both groups improved significantly after nursing. A much greater improvement was seen in the study group than in the control group. This suggests that this model can effectively increase social support for mothers. Relevant clinical studies have shown that the application of a humanized nursing model can significantly improve maternal compliance, reduce the incidence of adverse events in the postpartum period, and improve nursing satisfaction[22]. Studies have shown[23] that most mothers experience adverse events such as increased blood pressure, increased heart rate and sleep disturbance due to negative emotions, all of which may be unfavorable for childbirth. The results showed that the rate of cesarean deliveries, neonatal asphyxia and postpartum hemorrhage among patients in the study group were lower than those of patients in the control group. Also, the rate of nursing satisfaction of patients in the study group was significantly higher than that of patients in the control group. These two findings suggest that the humanized nursing model based on the use and gratification theory can improve pregnancy outcomes and improve nursing satisfaction.
It must be stated that this study has limitations of its own, namely the small sample size, short observation period and lack of long-term follow-up. It is hoped that future studies with larger sample sizes, longer observation periods and long-term follow-up may be carried out to arrive at more accurate and definite conclusions.
5 CONCLUSION
The humanized nursing model in obstetric nursing based on the use and gratification theory is a reliable strategy in obstetric nursing. It can reduce postpartum anxiety and depression, enhance self-efficacy and social support, improve pregnancy outcomes and increase nursing satisfaction. It has created a new concept for the care of obstetric patients. It is hoped that more health personnel can promote and apply this nursing model in the course of healthcare provision.
Acknowledgements
Not applicable.
Conflicts of Interest
The authors declared to have no conflict of interest.
Author Contribution
Both authors contributed to the manuscript and approved the final version.
Abbreviation List
BMI, Body mass index
EE-16, Efficiency expectation
EPDS, Edinburgh postnatal depression scale
GSES-C32, General self-efficacy scale
OE-16, Outcome expectation
SSS, Social support scale
References
[1] Uguz F, Gezginc K, Korucu DG et al. Are major depression and generalized anxiety disorder associated with oligohydramnios in pregnant women? A case-control study. Perspect Psychiatr C, 2017; 53: 275-279. DOI: 10.1111/ppc.12174
[2] Kim BN, Kwon SM. Initial Psychometric properties of the korean altman self-rating mania scale: Preliminary validation study in a non-clinical sample. Psychiat Invest, 2017; 14: 562-567. DOI: 10.4306/pi.2017.14.5.562
[3] Sunnqvist C, Sjöström K, Finnbogadóttir H. Depressive symptoms during pregnancy and postpartum in women and use of antidepressant treatment-a longitudinal cohort study. Int J Women’s Health, 2019; 11: 109-117. DOI: 10.2147/IJWH.S185930
[4] Rehman B, Ahmad J, Rashid K et al. An epidemiological study to assess the mental health status of pregnant women in a tertiary care hospital, Srinagar, Jammu and Kashmir, India. Int J Reprod Contracept Obstet Gynecol, 2017; 6: 2580-2583.
[5] Dagvadorj A, Ganbaatar D, Balogun O et al. Maternal socio-demographic and psychological predictors for risk of developmental delays among young children in Mongolia. BMC Pediatr, 2018; 18: 68-70. DOI: 10.1186/s12887-018-1017-y
[6] Petrozzi A, Gagliardi L. Breastfeeding self-efficacy scale: Validation of the italian version and correlation with breastfeeding at 3 months. J Pediatr Gastr Nutr, 2016; 62: 137-139. DOI: 10.1097/MPG.0000000000000902
[7] Xia CJ. Influence of lateral decubitus delivery on delivery outcomes based on humanized nursing [In Chinese]. Chinese Med Clin Med, 2019; 19: 821-823. DOI: 10.11655/zgywylc2019.05.060
[8] Bu N. Observation on the effect of humanized nursing on improving nursing quality in obstetrics and delivery room [In Chinese]. Chinese Med Gu, 2022; 20: 26-29.
[9] Shrestha SD, Pradhan R, Tran TD et al. Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower middle-income countries: A systematic review. BMC Pregnancy Child, 2016; 16: 1-19. DOI: 10.1186/s12884-016-0859-2
[10] Ghorat F, Esfehani RJ, Sharifzadeh M et al. Long term effect of vaginal delivery and cesarean section on female sexual function in primipara mothers. Electron Physician, 2017; 9: 3991-3996. DOI: 10.19082/3991
[11] Yazdanimehr R, Omidi A, Sadat Z et al. The Effect of mindfulness-integrated cognitive behavior therapy on depressionand anxiety among pregnant women: A randomized clinical trial. J Caring Sci, 2016; 5: 195-204. DOI: 10.15171/jcs.2016.021
[12] Yee LM, Martinez NG, Nguyen AT et al. Using a patient navigator to improve postpartum care in an urban women's health clinic. Obstet Gynecol, 2017; 129: 925-933. DOI: 10.1097/AOG.0000000000001977
[13] Mori E, Tsuchiya M, Maehara K et al. Fatigue, depression, maternal confidence, and maternal satisfaction during the first month postpartum: A comparison of Japanese mothers by age and parity. Int J Nurs Pract, 2017; 23: e12508. DOI: 10.1111/ijn.12508
[14] Hoekzema E, Barba-Müller E, Pozzobon C et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci, 2017; 20: 287-296. DOI: 10.1038/nn.4458
[15] Abraji NN. Exploring the application effect of humanized nursing in obstetrics and gynecology nursing. World Latest Med Inform Digest, 2019; 19; 301: 303.
[16] Li Y. The effect of humanized nursing mode on the psychological state and rehabilitation of patients with ovarian cyst pedicle torsion in the second and third trimesters of pregnancy [In Chinese]. Prim Med Forum, 2022; 26: 85-87.
[17] Medeiros RMK, Teixeira RC, Nicolini AB et al. Humanized care: The insertion of obstetric nurses in a teaching hospital [In Portuguese]. Revista Brasileira de Enfermagem, 2017; 69: 1091-1098. DOI: 10.1590/0034-7167-2016-0295
[18] Li C, Li Q, Li X. Effects of comprehensive nursing intervention on maternal self-efficacy and childbirth [In Chinese]. J Pract Clin Med, 2016; 20: 204-205.
[19] Yang W, Wang L, An X et al. Effects of midwifery-based comprehensive intervention on maternal self-efficacy and childbirth outcome [In Chinese]. J Chinese People’s Liberation Army, 2016; 33: 24-27.
[20] Sun C, Guo D. Observation on the application effect of humanized nursing in obstetrics and gynecology nursing [In Chinese]. Chinese Foreign Women's Health Res, 2019; 8: 67-68.
[21] Ertel KA, Huang T, Rifas-Shiman SL et al. Perinatal weight and risk of prenatal and postpartum depressive symptoms. Ann Epidemiol, 2017; 27: 695-700. DOI: 10.1016/j.annepidem.2017.10.007
[22] Li J. Study on the Value of Humanized Service in Obstetrics and Gynecology Nursing [ In Chinese]. Gu China Med, 2019; 17: 235-236.
[23] Barkin JL, Wisner KL, Bromberger JT et al. Factors associated with postpartum maternal functioning in women with positive screens for depression. J Women’s Health, 2016; 25: 707-713. DOI: 10.1089/jwh.2015.5296
Copyright © 2022 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.





 Copyright ©
Copyright ©