Effect of Humanistic Nursing on Preoperative Anxiety, Postoperative Pain Relief and Prognosis of Colorectal Cancer Patients
Jing Liang1, Xiaofeng Tian2, Wei Yang2*
1Department of Gastro-colorectal surgery, China-Japan Union Hospital of Jilin University, Changchun, Jilin Province, China
2Department of Hepatobiliary and Pancreatic Surgery, China-Japan Union Hospital of Jilin University, Changchun, Jilin Province, China
*Correspondence to: Wei Yang, China-Japan Union Hospital of Jilin University, 126 Sendai Dajie, Changchun 130000, Jilin, China; email: jlccyangwei@jlu.edu.cn
Abstract
Objective: This research aimed to probe into the effect of humanistic nursing on preoperative anxiety, postoperative pain relief and prognosis of colorectal cancer (CRC) patients.
Methods: Ninety-eight CRC patients who received surgical treatment in our hospital from January 2018 to June 2019 were selected as the research participants. They were randomized into observation group (OG) and control group (CG). The former was given humanistic nursing while the latter was given routine nursing. The preoperative and postoperative psychological condition, treatment effect, nursing satisfaction, VAS score after nursing, occurrence of complications, postoperative recovery and relevant serum indexes of patients were evaluated.
Results: Before surgery, there was no marked difference between both groups (P>0.05). While after surgery, patients in the OG had good treatment effect and high nursing satisfaction, and their VAS scores were dramatically lower than those in the CG. The postoperative psychological condition including self-evaluation and other evaluation anxiety and depression scores were also obviously lower than those in the CG. Serum related indexes such as CD3+, CD4+, CD8+ T lymphocyte and albumin levels were dramatically better than those of the CG, and plasma motilin level was also optimized dramatically. The diamine oxidase, D-lactic acid and lipopolysaccharide levels were the functional indexes of intestinal wall barrier, which were also obviously lower than those of the CG. The incidence of postoperative complications in the OG was low (P<0.05).
Conclusion: Humanistic nursing is a kind of nursing method worthy of promotion for relieving postoperative anxiety and depression of CRC patients, reducing postoperative pain and improving prognosis.
Keywords: humanistic nursing, colorectal cancer, anxiety, pain, prognosis effect
1 Introduction
Colorectal cancer (CRC) is a familiar malignancy, including colon cancer and rectal cancer[1]. The morbidity from high to low is successively rectum, sigmoid colon, cecum, ascending colon, descending colon and transverse colon. Recently, it tends to develop towards proximal end (right colon). Its incidence is relevant to lifestyle, heredity and colorectal adenoma[2]. At the moment, there are surgical treatment, chemotherapy, radiotherapy and traditional Chinese medicine treatment. Surgical resection of cancer is the main treatment scheme, and about 80% CRC patients receive surgical treatment[3]. Recently, the survival and remission rates of CRC patients have been greatly improved due to the improvement of the comprehensive treatment level of tumors. However, due to the influence of enterostomy and the absence and abnormality of intestinal function, many patients have developed various psychological diseases after surgery. It affects their body and mind even more than the disease itself; meanwhile, it also reduces the immune function of the body and affects the quality of life[4]. Quality of life refers to a person’s functional ability and subjective feeling in society and daily life, and it is a comprehensive concept including biomedicine and social psychology[5]. With the change of health concept, the quality of life has become a recognized efficacy evaluation index[6]. Therefore, the humanistic nursing mode is adopted clinically to carry out unified nursing intervention on the physical and psychological condition, so as to improve recovery effect, correct physical and mental state and enhance body immunity[6].
With the rapid changes in economy and people’s living standards, people’s health concepts and requirements for clinical nursing services have also changed to some extent. Routine nursing is applied to general surgery nursing, and the effect is satisfactory. But some patients are prone to negative emotions due to poor self-regulation ability. Humanistic nursing is based on modern nursing concept. This nursing method adheres to the principle of people-oriented, advocates taking patients as the center, and creates a comfortable and warm environment for patients through sincere, careful and patient service, so as to obtain a good prognosis. Thus, its application in clinical nursing of general surgery can effectively improve their nursing satisfaction[7,8].
This research mainly discusses the effect of applying humanistic nursing mode to the perioperative period of CRC patients on improving preoperative anxiety, postoperative pain and prognosis.
2 Materials and methods
2.1 Objects of Research
Ninety-eight CRC patients who received surgical treatment in our hospital from January 2018 to June 2019 were selected as the research participants. They were randomized into observation group (OG) and control group (CG). There were 56 cases in the OG, including 33 males and 23 females, aged (65.4±5.5); while there were 42 cases in the CG, including 24 males and 18 females, aged (65.7±5.2). The general data of patients were comparable (Table 1). Inclusion criteria were as follows: those confirmed as CRC by histopathological diagnosis; those with no contraindications for surgery; those suitable for surgical treatment exclusion criteria; patients with distant metastasis (such as liver and lung metastasis, etc.); patients who could not express their wishes accurately or could not cooperate with the questionnaire survey due to their own reasons. All patients were informed of the treatment and nursing plans, and their families signed consent forms. Besides, those complicated with tumors of other organs were excluded.
Table 1. General Data
|
CG (n=42) |
OG (n=56) |
χ2/t |
P value |
Gender [n(%)] |
|
|
|
|
Male |
24 |
33 |
0.0314 |
0.8592 |
Female |
18 |
23 |
|
|
Age (years) |
65.7±5.2 |
65.4±5.5 |
0.2734 |
0.7851 |
BMI (kg/m2) |
21.3±2.5 |
21.5±2.2 |
0.4151 |
0.6790 |
Cardiovascular diseases [n(%)] |
|
|
0.1050 |
0.7460 |
Yes |
7 |
8 |
|
|
No |
35 |
48 |
|
|
Diabetes [n(%)] |
|
|
0.0471 |
0.8282 |
Yes |
9 |
11 |
|
|
No |
33 |
45 |
|
|
Hypertension [n(%)] |
|
|
0.0653 |
0.7983 |
Yes |
13 |
16 |
|
|
No |
29 |
40 |
|
|
Degree of differentiation |
|
|
0.1237 |
0.7250 |
Highly and moderately differentiated |
24 |
30 |
|
|
Poorly differentiated |
18 |
26 |
|
|
Clinical staging |
|
|
0.0034 |
0.9532 |
I-II |
19 |
25 |
|
|
III |
23 |
31 |
|
|
2.2 Methods
CG: Routine perioperative professional nursing measures were adopted for CRC surgery.
OG: On the basis of the CG, humanistic nursing mode was adopted: health education: targeted explanation of relevant knowledge, characteristics and countermeasures to CRC surgery patients and their families, and provision of necessary medical and nursing guidance, such as medication principles, diet guidance, disease prevention, etc. Psychological intervention: from the point of view of psychological medicine, the medical workers should explain the influence of emotion on treatment to patients undergoing CRC surgery, guide them to learn self-control and emotion regulation, and always receive treatment with good mentality. Any efforts and progress made by patients undergoing CRC surgery should be determined and encouraged, so that they could feel their self-worth and face difficulties and challenges with full confidence. To minimize their worries, psychological counseling should be considered when necessary, so as to eliminate negative emotions. Evidence-based nursing: evidence-based nursing should be applied throughout the perioperative period of CRC surgery patients.
2.3 Outcome Measures
The efficacy, nursing satisfaction, VAS score after nursing, complications and postoperative recovery were compared between the two groups. Immunological indexes: peripheral blood of patients were collected at the time of admission and 3 days after surgery, and the levels of CD3+, CD4+, CD8+ T lymphocyte and albumin in serum and plasma motilin were tested via flow cytometry. Diamine oxidase (DAO), D-lactic acid (D-LAC) and lipopolysaccharide (LPS) were detected as functional indexes of intestinal wall barrier. The depression and anxiety of patients before and 2 months after discharge from hospital (self-rating) were evaluated by self-rating depression scale (SDS) and self-rating anxiety scale (SAS). SDS and SAS ≥50 points indicated that patients were accompanied by depression and anxiety symptoms, and the higher the score was, the more serious the depression and anxiety was. The anxiety and depression of patients before surgery and 2 months after discharge from hospital (other evaluation) were evaluated by Hamilton anxiety scale (HAMA) and Hamilton depression scale (HAMD). If the scores of both were greater than 18, they were positive. Patients’ quality of life before surgery and 2 months after discharge was assessed. It has 100 points for each item, and the score is directly proportional to the quality of life.
2.4 Statistical analysis
The data were processed by SPSS21.0, and the measurement data were expressed as the mean±standard deviation of at least three independent experiments. The comparison between groups was analyzed through t test. The counting data were expressed as (n, %) and analyzed and plotted through chi-square test and GraphPad Prism 6.
3 Results
3.1 Comparison of Efficacy and Nursing Satisfaction of Patients Between Both Groups
The effective rate of treatment in the OG was dramatically higher than that in the CG, and patients’ satisfaction with nursing was also obviously better (P<0.05) (Tables 2 and 3).
Table 2. Comparison of Efficacy of Patients in Both Groups
|
Markedly Effective |
Effective |
Ineffective |
Total Effective Rate (Markedly Effective+Effective) |
CG (n=42) |
11(26.2) |
23(54.8) |
8(19.0) |
34(83.3) |
OG (n=56) |
22(39.3) |
31(55.4) |
3(5.3) |
53(94.7) |
χ2/t |
|
|
|
4.5141 |
P |
|
|
|
0.0336 |
Table 3. Comparison of Nursing Satisfaction of Patients Between Both Groups
|
Very Satisfied |
Satisfied |
Dissatisfied |
Total Satisfaction Rate (Very Satisfied+Satisfied) |
CG (n=42) |
15(35.7) |
20(47.6) |
7(16.7) |
35(83.3) |
OG (n=56) |
25(44.6) |
29(51.8) |
2(3.6) |
54(96.4) |
χ2/t |
|
|
|
4.9351 |
P |
|
|
|
0.0263 |
3.2 Comparison of Postoperative Recovery of Patients in Both Groups
By comparing the postoperative recovery of patients in both groups, we found that the observation indexes included recovery time of bowel sounds, anal exhaust, eating, first defecation and hospitalization. The index time of patients in the OG was dramatically shorter than that in the CG (P<0.0001) (Table 4).
Table 4. Comparison of Postoperative Recovery of Patients Between Both Groups
|
Recovery Time of Bowel Sounds (h) |
Anus Exhaust Time (h) |
Eating Time (h) |
First Defecation Time (d) |
Length of Stay (d) |
CG (n=42) |
22.43±3.98 |
36.73±5.31 |
35.64±5.12 |
3.82±1.43 |
13.86±3.65 |
OG (n=56) |
15.92±3.07 |
26.13±4.85 |
24.38±4.96 |
2.52±1.19 |
9.12±2.75 |
χ2/t |
9.1439 |
10.2798 |
10.9690 |
4.9068 |
7.3349 |
P |
<0.0001 |
<0.0001 |
<0.0001 |
<0.0001 |
<0.0001 |
3.3 VAS Scores of Patients in Both Groups After Nursing
We compared the postoperative pain of patients in both groups. From the VAS scores of 1, 2, 3 and 5 days after surgery, it could be concluded that the pain scores of patients in the OG were dramatically lower than those in the CG at each time point (P<0.001) (Table 5).
Table 5. VAS Scores of Patients in Both Groups After Nursing
|
One Day After Surgery |
Two Days After Surgery |
Three Days After Surgery |
Five Days After Surgery |
CG (n=42) |
3.98±0.82 |
3.34±0.72 |
3.05±0.71 |
2.53±0.48 |
OG (n=56) |
3.05±0.81 |
2.78±0.79 |
2.03±0.67 |
1.45±0.38 |
χ2/t |
5.5952 |
3.6055 |
7.2697 |
12.4318 |
P |
<0.0001 |
0.0004 |
<0.0001 |
<0.0001 |
3.4 Postoperative Immunological Indexes of Patients in Both Groups
Before nursing intervention, the levels of CD3+, CD4+, CD8+ and CD4+/CD8+ in both groups had no remarkable difference (P>0.05). While after nursing intervention, the levels of CD3+, CD4+ and CD4+/CD8+ in the OG were higher than those in the CG, and the CD8+ level was lower than that in the CG, with statistically obvious differences (P<0.05) (Table 6).
Table 6. Postoperative Immunological Indexes of Patients in Both Groups
|
CD3+ (%) |
CD4+ (%) |
CD8+ (%) |
CD4+/CD8+ |
||||
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
Before Nursing |
After Nursing |
|
CG (n=42) |
59.91±17.7 |
63.8±18.1 |
35.6±7.45 |
42.9±9.13 |
28.7±8.76 |
23.4±6.56 |
1.24±0.42 |
1.83±0.72 |
OG (n=56) |
60.22±18.2 |
76.5±16.5 |
36.2±8.01 |
49.4±10.03 |
29.2±8.54 |
20.1±6.02 |
1.23±0.36 |
2.45±1.09 |
χ2/t |
0.0844 |
3.6169 |
0.3780 |
3.2978 |
0.2837 |
2.5840 |
0.1267 |
3.1979 |
P |
0.9329 |
0.0005 |
0.7063 |
0.0014 |
0.7773 |
0.0113 |
0.8995 |
0.0019 |
3.5 Comparison of Intestinal Wall Barrier Function Index, Motilin Level and Albumin Index of Patients in Both Groups
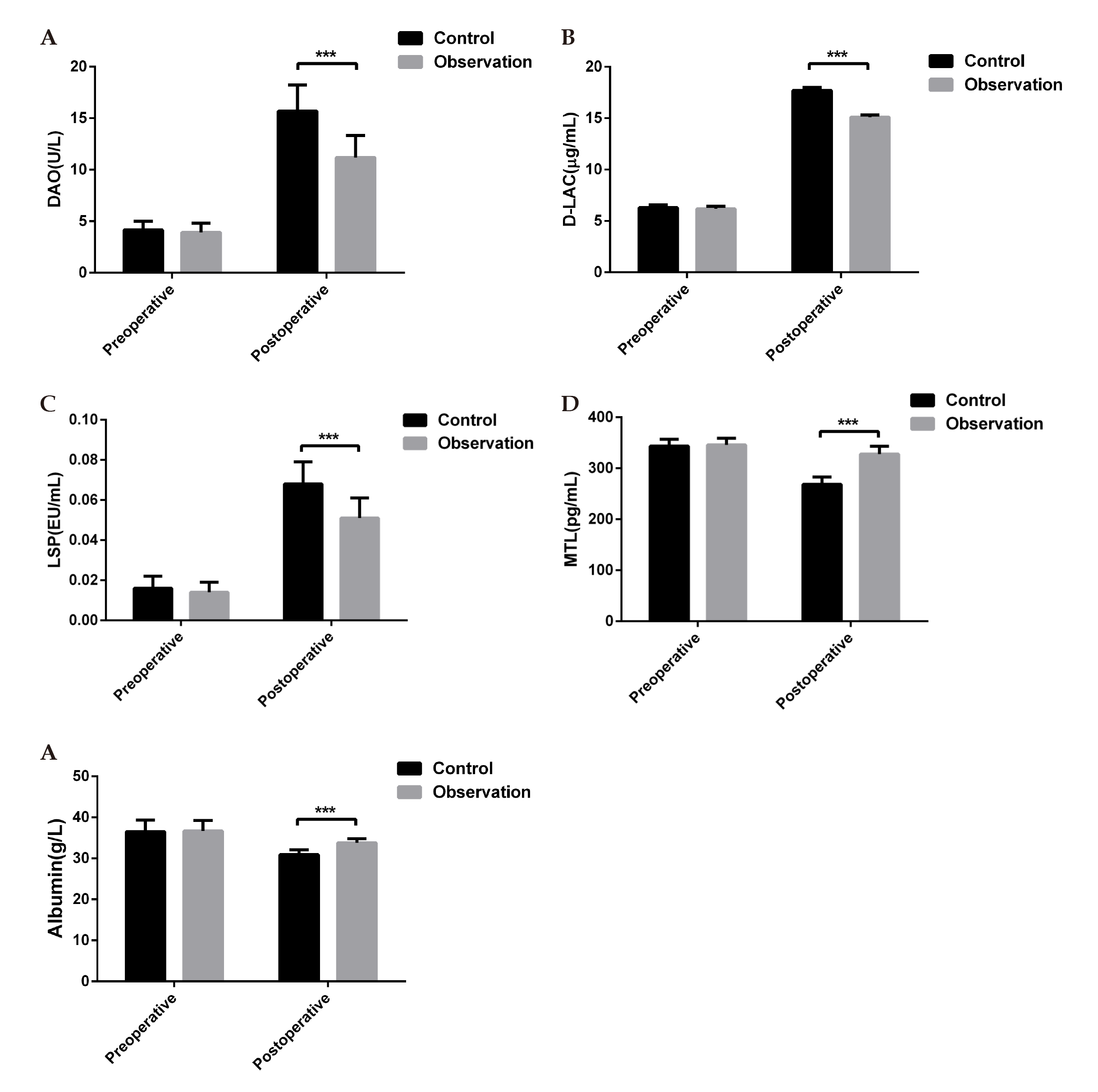
By comparing the intestinal wall barrier function and the levels of motilin and albumin of patients in both groups, we found that there was no statistically marked difference in each index before surgery (P>0.05). While after surgery, the levels of diamine oxidase (DAO), D-lactic acid (D-LAC) and lipopolysaccharide (LPS) in the OG were lower than those in the CG; the levels of motilin and albumin were higher than those of the CG, and the difference was statistically obvious (P<0.0001) (Figure 1).
|
Figure 1. Comparison of intestinal wall barrier function index, motilin level and albumin index of patients in both groups. A: Comparison of DAO levels between both groups before and after surgery; B: Comparison of D-LAC levels between both groups before and after surgery; C: Comparison of LSP level between both groups before and after surgery; D: Comparison of MTL level between both groups before and after surgery; E: Comparison of albumin levels between both groups before and after surgery). ***Indicates the comparison with CG (P<0.0001).
3.6 Comparison of Depression and Anxiety Scores of Patients in Both Groups
The mental states of the two groups were evaluated by themselves and others before operation and 2 months after discharge. The results showed that there was no remarkable difference in SAS, SDS, HAMA and HAMD scores before surgery (P>0.05). Two months after discharge, the scores of all indexes in the OG were lower than those in the CG, and the difference was statistically remarkable (P<0.0001). This revealed that the psychological condition of patients in the OG was remarkably better than that in the CG (Table 7).
Table 7. Comparison of Depression and Anxiety Scores of Patients in Both Groups
|
SAS Scores |
SDS Scores |
HAMA Scores |
HAMD Scores |
||||
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
|
CG (n=42) |
59.66±5.15 |
29.94±5.01 |
56.86±5.06 |
30.29± 4.81 |
23.56±3.51 |
14.56±3.01 |
21.67±3.32 |
13.43±4.02 |
OG (n=56) |
60.22±5.21 |
23.82±4.32 |
57.42±5.09 |
22.91±3.16 |
22.93±3.58 |
10.67±2.67 |
21.34±3.15 |
9.34±4.12 |
χ2/t |
0.5292 |
6.4793 |
1.3895 |
9.1532 |
1.0073 |
6.7573 |
0.5015 |
4.9139 |
P |
0.5979 |
<0.0001 |
0.1679 |
<0.0001 |
0.3163 |
<0.0001 |
0.6172 |
<0.0001 |
3.7 Quality of Life of Patients in Both Groups
The difference of quality of life of patients between the two groups before surgery and 2 months after discharge was compared, mainly from the aspects of physical condition, physiological function, emotional state, social function, self-ability and mental health. There was no obvious difference in the scores of various indexes before surgery (P>0.05). Two months after discharge, the scores of various indexes in the OG were dramatically better than those in the CG (P<0.001), indicating that the quality of life in the OG was better (Table 8).
Table 8. Quality of life of Patients in Both Groups
Physical Condition |
Physiological Function |
Emotional State |
||||
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
|
CG (n=42) |
28.6±6.3 |
36.8±6.9 |
38.9±12.8 |
47.7±14.4 |
26.2±10.3 |
37.8±11.2 |
OG (n=56) |
27.8±7.1 |
46.2±7.8 |
38.2±12.5 |
60.9±11.3 |
25.8±10.8 |
46.2±10.2 |
χ2/t |
0.5789 |
6.1988 |
0.2715 |
5.0852 |
0.1851 |
3.8681 |
P |
0.5640 |
<0.0001 |
0.7866 |
<0.0001 |
0.8536 |
0.0001 |
|
|
|
|
|
|
|
|
Social Function |
Self-ability |
Mental Health |
|||
|
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
Before Surgery |
Two Months After Discharge From Hospital |
CG (n=42) |
48.8±11.2 |
59.4±14.3 |
38.5±6.8 |
44.9±7.3 |
55.8±9.2 |
69.4±11.9 |
OG (n=56) |
47.9±10.9 |
71.3±11.9 |
38.1±6.3 |
57.2±8.2 |
54.1±8.9 |
75.9±11.2 |
χ2/t |
0.3998 |
4.4916 |
0.3006 |
7.6974 |
0.9224 |
2.7680 |
P |
0.6802 |
<0.0001 |
0.7643 |
<0.0001 |
0.3587 |
0.0068 |
3.8 Comparison of Complications
In the CG, there were 2 cases of vomiting (4.76%), 3 abdominal pain (7.14%), 3 abdominal distension (7.14%), and 2 intestinal fistula (4.76%); while in the OG, there were 1 case of vomiting (1.78%), 2 abdominal pain (3.57%), 1 abdominal distension (1.78%), and 1 intestinal fistula (1.78%). The incidence of vomiting, abdominal pain, abdominal distension and intestinal fistula in the OG were dramatically lower than those in the CG, the difference was statistically marked (P<0.05) (Table 9).
Table 9. Comparison of Incidence of Complications of Patients Between Both Groups
|
Vomiting |
Abdominal Pain |
Abdominal Distension |
Intestinal Fistula |
Total Incidence Rate |
CG (n=42) |
2(4.76) |
3(7.14) |
3(7.14) |
2(4.76) |
10(23.8) |
OG (n=56) |
1(1.78) |
2(3.57) |
1(1.78) |
1(1.78) |
5(8.91) |
χ2/t |
|
|
|
|
4.1001 |
P |
|
|
|
|
0.0429 |
4 Discussion
Although CRC is a malignancy, with the development of medical technology, it can be cured without recurrence based on correct treatment and nursing[9]. However, because cancer has brought great fear to people for many years, patients have tension, fear and other psychology during and after treatment, and the unclear understanding of perioperative period has affected the efficacy. Hence, psychological depression is one of the vital indicators to evaluate the recovery of patients[10]. Humanistic nursing is to adopt targeted nursing intervention methods according to the specific conditions of postoperative patients, and to promote their psychological and physiological rehabilitation. Hence, it achieves the best self-condition and promotes the recovery of trauma[11].
This research compares the relief of psychological, physiological and prognostic effects of routine and humanistic nursing on CRC patients. The results show that the humanistic nursing group has good treatment effect and high nursing satisfaction, and the VAS score is dramatically lower than that of routine nursing group. Perioperative pain nursing is a vital nursing content for CRC patients. Appropriate drug treatment should be given for pain, but more is to communicate with patients. So, they can understand that pain is an inevitable process. Under the careful care of the hospital, pain will gradually disappear. During this process, patients should be given necessary psychological nursing, so that they can maintain emotional stability, actively cooperate with nursing staff, and accelerate recovery[12,13]. The psychological condition of patients in the humanistic nursing group including self-evaluation and other evaluation of anxiety and depression scores were also remarkably lower than those in the routine nursing group. Compared with routine nursing, humanistic nursing pays attention to the comprehensiveness and detail of nursing and the communication with patients. Thus, it can improve the mood of patients, meet their basic life and psychological needs, and improve their treatment and nursing compliance[14]. Simultaneously, the serum related indexes such as CD3+, CD4+, CD8+ T lymphocyte and albumin levels were remarkably better than those in the routine nursing group. Malignant tumor patients often have abnormal and disordered immune function, resulting in immunosuppression[15] and immune escape[16] of malignancy cells, avoiding the killing of immune cells in the body. However, the anti-tumor immunity of the body is mainly cellular and humoral immunity, which are jointly completed by lymphocyte subsets and immunoglobulin[17,18]. T cells are the main cellular immune molecules of the body, of which CD8+ T cells belong to inhibitory T lymphocytes, and the mechanism is to inhibit the cellular immunity mediated by auxiliary T lymphocytes[19]; CD4+ T cells are auxiliary T lymphocytes, which can enhance the cellular immune function of the body[20]; CD3+ T cells also belong to T lymphocytes, indicating the immune function of human cells[21]. Studies have shown that various nursing methods can improve the immune function of CRC patients[22]. Plasma motilin levels were also dramatically optimized. The levels of diamine oxidase, D-lactic acid and lipopolysaccharide were the functional indexes of intestinal wall barrier. And they were also obviously lower than those of the CG. Intestinal barrier function is a crucial natural protective barrier for the body[23]. Among the mechanical, immune, biological and chemical barriers of intestinal mucosa, mechanical one is the most critical[24]. It is the basis for intestinal barrier to function. When intestinal mucosal cell connection is broken and permeability is increased, DAO, D-LAC and LPS located in intestinal villi and lumen can enter blood through the damaged mechanical barrier; hence, the levels of DAO, D-LAC and LPS in peripheral blood increase[25]. Finally, the incidence of postoperative complications in the humanistic nursing group is low. In order to prevent patients from secondary infection, regular disinfection and cleaning are required. In detail, humanistic nursing will make different nursing plans in view of the different conditions of patients to reduce the occurrence of postoperative complications.
5 Conclusion
To sum up, humanistic nursing program can effectively improve patients’ bad psychological condition, relieve postoperative pain, promote postoperative body recovery, and improve the surgical treatment effect. It is quite remarkable to the development of clinical nursing work.
Acknowledgements
Not applicable.
Conflicts of Interest
These authors declared no conflict of interest.
Author Contribution
Yang W designed this study; Liang J and Yang W wrote the article; Liang J and Tian X collected the data and performed the statistical analysis; Tian X reviewed the manuscript; all authors approved the final version.
Abbreviation List
CG, Control group
CRC, Colorectal cancer
DAO, Diamine oxidase
D-LAC, D-lactic acid
HAMA, Hamilton anxiety scale
HAMD, Hamilton depression scale
LPS, Lipopolysaccharide
OG, Observation group
SAS, self-rating anxiety scale
SDS, Self-rating depression scale
References
[1] Siegel RL, Miller KD, Goding Sauer A et al. Colorectal cancer statistics, 2020. CA Cancer J Clin, 2020; 70: 145-164. DOI: 10.3322/caac.21601.
[2] Vermeer NC, Snijders HS, Holman FA et al. Colorectal cancer screening: Systematic review of screen-related morbidity and mortality. Cancer Treat Rev, 2017; 54: 87-98. DOI: 10.1016/j.ctrv.2017.02.002.
[3] Galli R, Rosenberg R. Surgical treatment of colorectal cancer. Ther Umsch, 2018; 75: 607-614. DOI: 10.1024/0040-5930/a001047.
[4] Brown JC, Damjanov N, Courneya KS et al. A randomized dose-response trial of aerobic exercise and health-related quality of life in colon cancer survivors. Psychooncology, 2018; 27: 1221-1228. DOI: 10.1002/pon.4655.
[5] Panzini RG, Mosqueiro BP, Zimpel RR et al. Quality-of-life and spirituality. Int Rev Psychiatry, 2017; 29: 263-282. DOI: 10.1080/09540261.2017.1285553.
[6] Xu S, Zhang Z, Wang A et al. Effect of self-efficacy intervention on quality of life of patients with intestinal stoma. Gastroenterol Nurs, 2018; 41: 341-346. DOI: 10.1097/SGA.0000000000000290.
[7] Perez-Fuentes MDC, Herrera-Peco I, Molero Jurado MDM et al. A cross-sectional study of empathy and emotion management: key to a work environment for humanized care in nursing. Front Psychol, 2020; 11: 706. DOI: 10.3389/fpsyg.2020.00706.
[8] Beltran Salazar OA. Humanized care: A relationship of familiarity and affectivity. Invest Educ Enferm, 2015; 33: 17-27. DOI: 10.17533/udea.iee.v33n1a03.
[9] Chakedis J, Schmidt CR. surgical treatment of metastatic colorectal cancer. Surg Oncol Clin N Am, 2018; 27: 377-399. DOI: 10.1016/j.soc.2017.11.010.
[10] Pitman A, Suleman S, Hyde N et al. Depression and anxiety in patients with cancer. BMJ, 2018; 361: k1415. DOI: 10.1136/bmj.k1415.
[11] Wu HL, Volker DL. Humanistic nursing theory: application to hospice and palliative care. J Adv Nurs, 2012; 68: 471-479. DOI: 10.1111/j.1365-2648.2011.05770.x.
[12] Nimmo SM, Foo ITH, Paterson HM. Enhanced recovery after surgery: Pain management. J Surg Oncol, 2017; 116: 583-591. DOI: 10.1002/jso.24814.
[13] Higgs S, Henry R, Glackin M. Acute pain services following surgery for colorectal cancer. Br J Nurs, 2014; 23: S4, S6, S8-11. DOI: 10.12968/bjon.2014.23.Sup2.S4.
[14] Beltran Salazar OA. The meaning of humanized nursing care for those participating in it: Importance of efforts of nurses and healthcare institutions. Invest Educ Enferm, 2016; 34: 18-28. DOI: 10.17533/udea.iee.v34n1a03.
[15] Axelrad JE, Lichtiger S, Yajnik V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J Gastroenterol, 2016; 22: 4794-4801. DOI: 10.3748/wjg.v22.i20.4794.
[16] Liu Y, Cao X. Immunosuppressive cells in tumor immune escape and metastasis. J Mol Med (Berl), 2016; 94: 509-522. DOI: 10.1007/s00109-015-1376-x.
[17] Hu Z, Zou Q, Su B. Regulation of T cell immunity by cellular metabolism. Front Med, 2018; 12: 463-472. DOI: 10.1007/s11684-018-0668-2.
[18] Kanellopoulos JM, Ojcius DM. Development of humoral immunity. Biomed J, 2019; 42: 207-208. DOI: 10.1016/j.bj.2019.08.003.
[19] Pilipow K, Scamardella E, Puccio S et al. Antioxidant metabolism regulates CD8+ T memory stem cell formation and antitumor immunity. JCI Insight, 2018; 3. DOI: 10.1172/jci.insight.122299.
[20] Hohman LS, Peters NC. CD4+ T cell-mediated immunity against the phagosomal pathogen leishmania: Implications for vaccination. Trends Parasitol, 2019; 35: 423-435. DOI: 10.1016/j.pt.2019.04.002.
[21] Oba R, Isomura M, Igarashi A et al. Circulating CD3+ HLA-DR+ Extracellular Vesicles as a Marker for Th1/Tc1-Type Immune Responses. J Immunol Res, 2019; 2019: 6720819. DOI: 10.1155/2019/6720819.
[22] Kelly DL, Lyon DE, Yoon SL et al. The microbiome and cancer: Implications for oncology nursing science. Cancer Nurs, 2016; 39: E56-62. DOI: 10.1097/NCC.0000000000000286.
[23] Xu Q, Xu P, Cen Y et al. Effects of preoperative oral administration of glucose solution combined with postoperative probiotics on inflammation and intestinal barrier function in patients after colorectal cancer surgery. Oncol Lett, 2019; 18: 694-698. DOI: 10.3892/ol.2019.10336.
[24] Ren Z, Guo C, Yu S et al. Progress in mycotoxins affecting intestinal mucosal barrier function. Int J Mol Sci, 2019; 20. DOI: 10.3390/ijms20112777.
[25] Liang FF, Wang J, Li L et al. Chronic liver disease increases with damage to intestinal barrier function. Zhonghua Gan Zang Bing Za Zhi, 2018; 26: 612-617. DOI: 10.3760/cma.j.issn.1007-3418.2018.08.010.
Copyright © 2021 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.




 Copyright ©
Copyright ©