Clinical Value of Comprehensive Nursing Intervention in Prevention of Ventilator-associated Pneumonia
Cuifang Liu1, Yumei Zhou2, Jingjing Zhao2, Nana Geng1*
2Pediatric Infusion Rooms, Shandong Dongying People's Hospital, Dongying, Shandong Province, China.
*Correspondence to: Nana Geng, Department of Respiratory Medicine, Shandong Dongying People's Hospital, Dongying 257000, Shandong Province, China; Email:185484833@qq.com
Abstract
Objective: To investigate the clinical value of comprehensive nursing intervention in prevention of ventilator-associated pneumonia.
Methods: From June 2018 to December 2019, a total of 116 patients who received mechanical ventilation were selected as research participants, and they were divided into control group (n=58) and observation group (n=58) according to the random number table method. In the observation group, patients were treated with comprehensive nursing, while patients in the control group were treated with conventional nursing. The mechanical ventilation time, hospitalization time, VAP incidence, psychological status, quality of life and nursing satisfaction of patients were compared in the two groups.
Results: The mechanical ventilation and hospitalization time of patients in the observation group were less than those of patients in the control group, and the difference was statistically significant (P<0.05). The incidence of VAP was 3.44% in the observation group, which was lower than that in the control group (13.79%), and the difference was statistically significant (P<0.05). The self-rating anxiety scale (SAS) and self-rating depression scale (SDS) scores of patients in the two groups before intervention were not of statistically significant difference (P>0.05). After intervention, the SAS and SDS scores decreased in the two groups, and the scores in the observation group were significantly lower than those in the control group (P<0.05). The quality of life scores before intervention between the two groups were not statistically significant (P>0.05). After intervention, the quality of life scores in the observation group were higher than those in the control group, and the difference was statistically significant (P<0.05). The nursing satisfaction rate in the observation group was 94.87%, which was significantly higher than that in the control group (81.03%) (P<0.05).
Conclusion: Comprehensive nursing intervention can shorten the time of mechanical ventilation and hospitalization, prevent the occurrence of VAP, alleviate the negative emotions of patients, and improve their quality of life as well as nursing satisfaction.
Keywords: comprehensive care, prevention, ventilator-associated pneumonia, clinical value
1 INTRODUCTION
Mechanical ventilation is one of the main rescue methods for respiratory failure, during which some patients often have some complications and ventilator-associated pneumonia (VAP) is one most common case[1,2]. VAP refers to pneumonia that develops after receiving mechanical ventilation treatment for 48 hours or within 48 hours after cessation of mechanical ventilation in the absence of pulmonary infection[3]. Patients with VAP complications may have difficulty in weaning, which prolongs hospital stay, seriously affects the quality of life and even threatens the life safety[4,5]. Therefore, it is vital to find an effective nursing method to prevent VAP during mechanical ventilation. This study aimed to explore the clinical value of comprehensive nursing intervention in the prevention of ventilator-associated pneumonia, so as to provide a clinical reference for the prevention of VAP. The results are reported as follows.
2 MATERIAL AND METHODS
2.1 General Material
From June 2018 to December 2019, a total of 116 patients admitted to our hospital for the treatment of mechanical ventilation were selected as study participants. This study was approved by the hospital’s Ethics Committee. According to the random number table method, the patients were divided into control group (n=58) and observation group (n=58). The general materials in the two groups were compared, and the difference was not statistically significant (P>0.05). See Table 1.
Table 1. Comparison of General Material
Group |
n |
Gender |
Average Age (years old) |
|
Male |
Female |
|||
Observation group |
58 |
32 |
26 |
|
Control group |
58 |
31 |
27 |
|
2/t |
|
0.035 |
0.360 |
|
P |
|
0.853 |
0.720 |
|
2.2 Methods
2.2.1 Control Group
In the control group, patients were treated with conventional nursing intervention, including conventional sputum suction nursing, posture nursing, psychological care and environmental nursing.
2.2.2 Observation Group
In the observation group, patients were treated with comprehensive nursing intervention on the basis of the control group. (1) Cognitive and psychological nursing: Patients on mechanical ventilation often had negative emotions such as anxiety and insecurity due to insufficient knowledge of mechanical ventilation. Nursing staff carries out detailed disease education for patients, explaining the purpose of the treatment and possible adverse reactions and making adequate psychological preparation for patients[6]. Patients were encouraged to actively face the disease and establish the confidence of treatment. (2) Environment and posture nursing: The indoor environment were kept ventilated, clean, and quiet with regular bacterial disinfection, while the temperature and humidity of the ward were controlled for a comfortable environment. According to patients’ condition, they were helped to be in a comfortable position with the head, neck and shoulders at the same level. To ensure the comfort of patients, they could tilt the head back and turn over regularly with help[7]. (3) Strengthening the nursing of respiratory tract: To ensure the airway patency of patients, the airway temperature and humidity of the patients were kept at an appropriate level, and the ventilator parameters were then adjusted according to their specific conditions. The correct way of spitting was explained to the patients, and the patients were assisted to turn over their bodies[8]. (4) Ventilator duct nursing: The ventilator pipes were replaced and the ventilators were cleaned in time to avoid cross-infection; The threaded pipe of the ventilator was changed every week, the condensed water in the respiratory pipe was cleaned in time, and antibiotics were used rationally; Intermittent weaning and early withdrawal of sedatives could reduce the incidence of VAP[9]. And (5) Nutritional support: According to the patients’ situation, appropriate diet plans were made; Nasal feeding was applied in patients who could not eat independently.
2.3 Observation Indexes
(1) Mechanical ventilation time and hospitalization time; (2) Incidence of VAP. (3) Psychological status: The self-rating anxiety scale (SAS)[10] was used for the evaluation, among which the severe anxiety score was >69, the moderate anxiety score was 60-69, the mild anxiety score was 50-59, and the normal score was <50. (2) Self-rating depression scale (SDS)[11] was used for scoring, among which severe depression score was >72 points, moderate depression score was 63-72 points, mild depression score was 53-62 points, and normal status score was <53 points. (4) Quality of life: The SF-36 scale[12] was used for evaluation, including psychology, emotion, body and society. The total score for each item was 100 points. The mean value of the four items was used to represent the quality of life. (5) Nursing satisfaction: Nursing satisfaction was evaluated according to the questionnaire designed by the nursing personnel. There were 8 items in total with five levels ranging from "very satisfied" to "very dissatisfied". The satisfaction rate = (very satisfied + satisfied + average)/number of cases ×100%.
2.4 Statistical Analysis
SPSS23.0 was used to process the collected data. The quantitative data that were consistent with normal distribution were expressed by x̅s. The qualitative data were expressed as n(%). The rank-sum test was performed for ordered qualitative data, while 2 test was used for the disordered data. The variance analysis was conducted for repeated measurement data. P<0.05 was considered significantly different.
3 RESULTS
3.1 Comparison of Mechanical Ventilation and Hospitalization Time
The time of mechanical ventilation and hospitalization in the observation group was less than that in the control group, and the difference was statistically significant (P<0.05). See Table 2.
Table 2. Comparison of Mechanical Ventilation and Hospitalization Time (x sd)
Group |
n |
Mechanical Ventilation Time |
Hospitalization Time |
Observation group |
58 |
||
Control group |
58 |
||
t |
|
8.966 |
6.876 |
P |
|
<0.001 |
<0.001 |
3.2 Comparison of VAP Incidence
The VAP incidence in the observation group was 3.44%, which was lower than that in the control group (13.79%), and the difference was statistically significant (P<0.05). See Table 3 for details.
Table 3. Comparison of VAP Incidence (n)
Group |
n |
With VAP |
Without VAP |
VAP Incidence |
Observation group |
58 |
2 |
56 |
3.44 |
Control group |
58 |
8 |
50 |
13.79 |
2 |
|
|
|
3.940 |
P |
|
|
|
0.047 |
3.3 Comparison of Psychological Status
The SAS and SDS scores of the two groups before intervention were not of significant difference (P>0.05). After intervention, the SAS and SDS scores decreased in both groups, while the scores in the observation group were lower than those in the control group and the difference was statistically significant (P<0.05). See Table 4 for details.
Table 4. Comparison of SAS and SDS Scores (x̅ s, score)
Group |
n |
SAS |
SDS |
||
Before Intervention |
After Intervention |
Before Intervention |
After Intervention |
||
Observation group |
58 |
||||
Control group |
58 |
||||
t |
|
0.130 |
14.301 |
0.533 |
4.707 |
P |
|
0.897 |
<0.001 |
0.595 |
<0.001 |
Notes: *stands for comparison with the data before intervention, P<0.05.
3.4 Comparison of Quality of Life
The quality of life scores of the two groups before intervention were not of significant difference (P>0.05). After intervention, the score in the observation group was higher than that in the control group, and the difference was statistically significant (P<0.05). See Table 5 for details.
Table 5. Comparison of Quality of Life (x̅ sd, score)
Group |
n |
Before Intervention |
After Intervention |
Observation group |
58 |
||
Control group |
58 |
||
t |
|
0.484 |
4.753 |
P |
|
0.629 |
<0.001 |
Notes: *stands for comparison with the data before intervention, P<0.05.
3.5 Comparison of Nursing Satisfaction
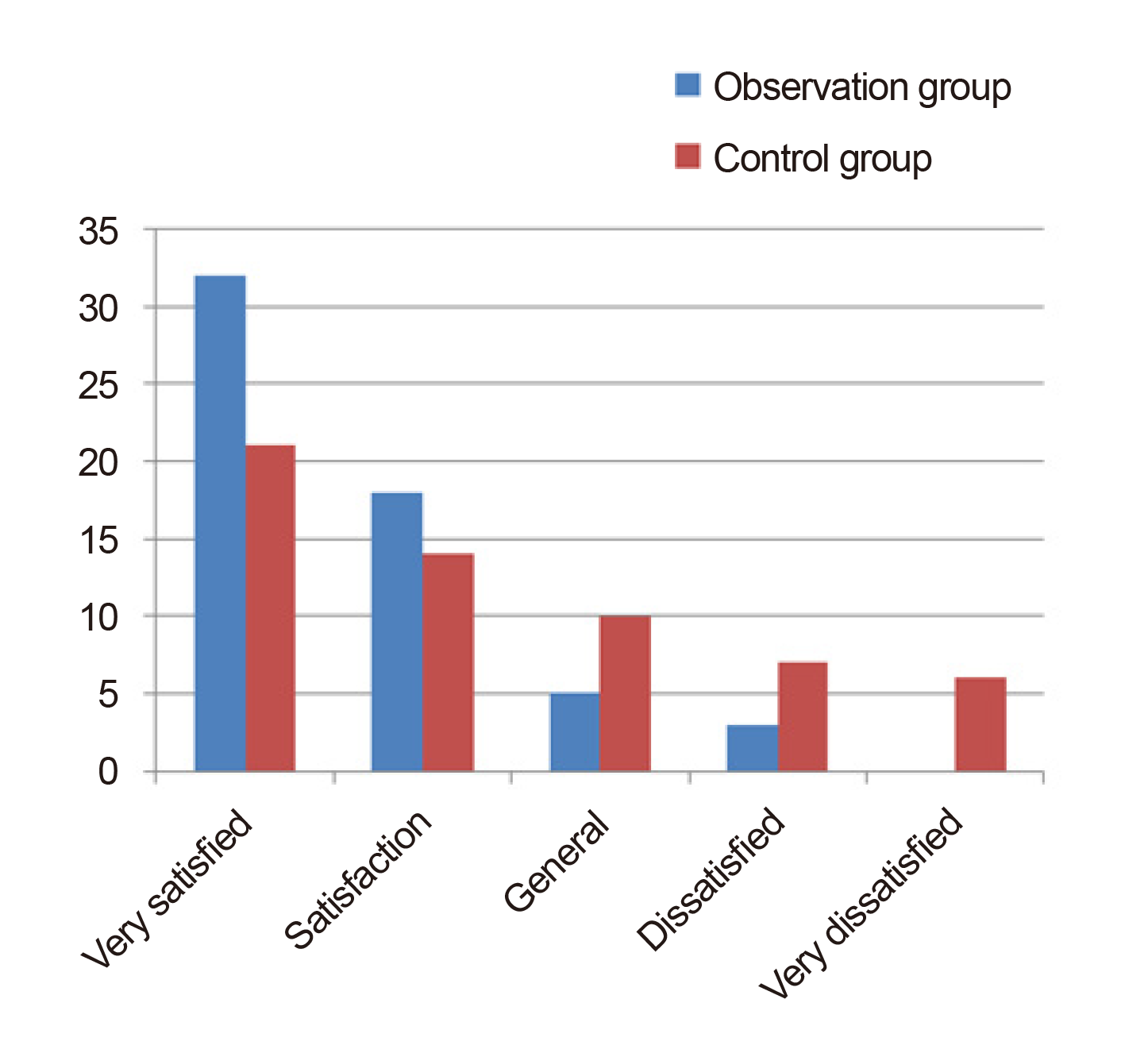
The nursing satisfaction in the observation group was 94.87%, which was higher than that in the control group (81.03%), and the difference was statistically significant (P<0.05). See Figure 1.
|
Figure 1. Comparison of nursing satisfaction between the two groups.
4 DISCUSSION
VAP is a common nosocomial infection, which is not only related to patients’ own disease[13], but also related to factors of antibiotic use, artificial airway, mistaken aspiration and mechanical ventilation time[14,15]. Among them, mechanical ventilation is an important reason for the development of VAP in patients. The longer the time of mechanical ventilation, the higher the incidence of VAP, which has a negative impact on the prognosis of patients[16]. VAP has a high mortality rate, so it is important to take appropriate prevention measures.
Comprehensive nursing intervention is a new patient-centered nursing model, which can effectively improve patients’ nursing services by utilizing various resources[17]. Cross-infection caused by foreign bacteria can be effectively avoided through environmental nursing in the wards[18]. After the patient's airway nursing, respiratory tract mucosal damage can be effectively avoided. Psychological nursing intervention can enhance patients' confidence in getting cured, improve patients' nursing and treatment compliance, and it is more conducive to the development of nursing work[19]. After ventilator tube nursing, the bacteria invasion can be effectively avoided in case of VAP. After comprehensive nursing, VAP can be prevented, mechanical ventilation and hospitalization time can be shortened, and patients' quality of life and nursing satisfaction can be improved[20]. The results of this study showed that the mechanical ventilation and hospitalization time in the observation group were less than those in the control group. The incidence of VAP in the observation group was 3.44%, which was lower than that in the control group (13.79%). The SAS and SDS scores in both groups were reduced after the intervention, and the scores in the observation group were lower than those in the control group. The nursing satisfaction in the observation group was 94.87%, which was higher than that in the control group (81.03%). The results showed that comprehensive nursing can effectively reduce mechanical ventilation time and hospitalization time, reduce the incidence of VAP, alleviate patients' negative emotions, and improve the quality of life as well as nursing satisfaction.
5 CONCLUSION
In conclusion, comprehensive nursing intervention can shorten mechanical ventilation time and hospitalization time, prevent the development of VAP, relieve patients’ negative emotions, and enhance their quality of life and nursing satisfaction.
Acknowledgements
Not applicable.
Conflicts of Interest
The authors declared no conflict of interest.
Author Contribution
Geng N designed this study and wrote the article; Liu C and Zhou Y collected the data and performed the statistical analysis; Zhao J revised the papers for important intellectual content; all authors approved the final version.
Abbreviation List
SAS, Self-rating anxiety scale
SDS, Self-rating depression scale
VAP, Ventilator-associated pneumonia
References
[1] Martinez-Ales G, Lopez-Cuadrado T, Olfson M et al. Use and outcomes of mechanical ventilation for people with severe mental disorders admitted due to natural causes: A nationwide population-based study. Gen Hosp Psychiatry, 2020; 65: 15-20. DOI: 10.1016/j.genhosppsych.2020.04.007.
[2] Jean R, Shah P, Yudelevich E et al. Effects of deep sedation on sleep in critically ill medical patients on mechanical ventilation. J Sleep Res, 2020; 29: e12894. DOI: 10.1111/jsr.12894.
[3] Huang D, Qi M, Hu Y et al. The impact of Candida spp airway colonization on clinical outcomes in patients with ventilator-associated pneumonia: A systematic review and meta-analysis. Am J Infect Control, 2020; 48: 695-701. DOI: 10.1016/j.ajic.2019.11.002.
[4] Shin JW, Tate JA, Happ MB. The facilitated sensemaking model as a framework for family-patient communication during mechanical ventilation in the intensive care unit. Crit Care Nurs Clin North Am, 2020; 32: 335-348. DOI: 10.1016/j.cnc.2020.02.013.
[5] Mutch WaC. Effects of variable versus non-variable controlled mechanical ventilation. Comment on Br J Anaesth 2020; 124: 430-9. Br J Anaesth, 2020; 124: e222-e223. DOI: 10.1016/j.bja.2020.02.010.
[6] Van Dijk SM, Hallensleben NDL, Van Santvoort HC et al. Acute pancreatitis: recent advances through randomised trials. Gut, 2017; 66: 2024-2032. DOI: 10.1136/gutjnl-2016-313595.
[7] Singh P, Garg PK. Pathophysiological mechanisms in acute pancreatitis: Current understanding. Indian J Gastroenterol, 2016; 35: 153-166. DOI: 10.1007/s12664-016-0647-y.
[8] Dos Santos FV, Cipriano G, Jr., Vieira L et al. Neuromuscular electrical stimulation combined with exercise decreases duration of mechanical ventilation in ICU patients: A randomized controlled trial. Physiother Theory Pract, 2020; 36: 580-588. DOI: 10.1080/09593985.2018.1490363.
[9] Osman S, Al Talhi YM, Aldabbagh M et al. The incidence of ventilator-associated pneumonia (VAP) in a tertiary-care center: Comparison between pre- and post-VAP prevention bundle. J Infect Public Health, 2020; 13: 552-557. DOI: 10.1016/j.jiph.2019.09.015.
[10] Dong X, Sun G, Zhan J et al. Telephone-based reminiscence therapy for colorectal cancer patients undergoing postoperative chemotherapy complicated with depression: a three-arm randomised controlled trial. Support Care Cancer, 2019; 27: 2761-2769. DOI: 10.1007/s00520-018-4566-6.
[11] Jokelainen J, Timonen M, Keinanen-Kiukaanniemi S et al. Validation of the Zung self-rating depression scale (SDS) in older adults. Scand J Prim Health Care, 2019; 37: 353-357. DOI: 10.1080/02813432.2019.1639923.
[12] Albayrak I, Biber A, Caliskan A et al. Assessment of pain, care burden, depression level, sleep quality, fatigue and quality of life in the mothers of children with cerebral palsy. J Child Health Care, 2019; 23: 483-494. DOI: 10.1177/1367493519864751.
[13] Harrell KN, Reynolds JK, Wilks GR et al. The effect of lung lavage volume return on the diagnosis of ventilator-associated pneumonia. J Surg Res, 2020; 248: 56-61. DOI: 10.1016/j.jss.2019.11.016.
[14] Portelli M, Jones CD. Severe acute pancreatitis: pathogenesis, diagnosis and surgical management. Hepatobiliary Pancreat Dis Int, 2017; 16: 155-159. DOI: 10.1016/s1499-3872(16)60163-7.
[15] Craven TH, Wojcik G, Mccoubrey J et al. Ventilator-associated pneumonia surveillance using two methods. J Hosp Infect, 2020; 104: 522-528. DOI: 10.1016/j.jhin.2020.01.020.
[16] Nesvaderani M, Eslick GD, Vagg D et al. Epidemiology, aetiology and outcomes of acute pancreatitis: A retrospective cohort study. Int J Surg, 2015; 23: 68-74. DOI: 10.1016/j.ijsu.2015.07.701.
[17] Maurya S, Mishra SB, Azim A et al. Ventilator-associated complications: A study to evaluate the effectiveness of a planned teaching program for intensive care unit staff nurses-an Indian experience. Am J Infect Control, 2016; 44: 1422-1423. DOI: 10.1016/j.ajic.2016.03.008.
[18] Jansson M, Ala-Kokko T, Ylipalosaari P et al. Critical care nurses' knowledge of, adherence to and barriers towards evidence-based guidelines for the prevention of ventilator-associated pneumonia-a survey study. Intensive Crit Care Nurs, 2013; 29: 216-227. DOI: 10.1016/j.iccn.2013.02.006.
[19] Iosifidis E, Stabouli S, Tsolaki A et al. Diagnosing ventilator-associated pneumonia in pediatric intensive care. Am J Infect Control, 2015; 43: 390-393. DOI: 10.1016/j.ajic.2015.01.004.
[20] Lim KP, Kuo SW, Ko WJ et al. Efficacy of ventilator-associated pneumonia care bundle for prevention of ventilator-associated pneumonia in the surgical intensive care units of a medical center. J Microbiol Immunol Infect, 2015; 48: 316-321. DOI: 10.1016/j.jmii.2013.09.007.
Copyright © 2021 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.





 Copyright ©
Copyright ©