Influence of Psychological Nursing Intervention Combined with Family-Like Care on Negative Emotion and Prognosis of Patients with Breast Cancer Undergoing Radical Mastectomy
Yunzhao Ji1*, Ning Yang2, Yanhua Zuo1
1Hebei PetroChina Central Hospital, Hebei Province, China
2People 's Hospital of CangZhou, Hebei Province, China
*Correspondence to: Yunzhao Ji, Bachelor, Hebei PetroChina Central Hospital, 51 Xinkai Road, Guangyang District, Langfang city, Hebei Province 065000, China; Email: mingzhi36932@163.com
Abstract
Objective: To explore the application effect of psychological nursing intervention combined with family-like care in patients with breast cancer undergoing radical mastectomy and analyze its influence on the prognosis and mental state.
Methods: A retrospective analysis was performed on 100 patients with breast cancer undergoing radical mastectomy in our hospital from September 2018 to September 2020. According to nursing methods, they were equally allocated to a control group and an experimental group. The control group received routine nursing, while the experimental group received psychological nursing intervention combined with family-like care. The following items of the two groups were compared: Nursing efficiency, nursing satisfaction, prevalence of adverse reactions, self-rating anxiety scale (SAS) scores, self-rating depression scale (SDS) scores, mental status scale in non-psychiatric settings (MSSNS) scores, Pittsburgh sleep quality index (PSQI) scores, quality of life index (QLI) scores, and incidence of negative emotions at 1, 2, 3 and 4 weeks after surgery.
Results: The experimental group scored higher than the control group in nursing efficiency, nursing satisfaction and QLI (all P<0.05), while it scored lower in the prevalence of adverse reactions, SAS, SDS, MSSNS, and the prevalence of negative emotions at 1, 2, 3 and 4 weeks after surgery (all P<0.05).
Conclusion: Psychological nursing intervention combined with family-like care significantly relieves the postoperative negative emotion and improves the prognosis, which has been unanimously recognized by patients. Therefore, this nursing model is of great value in practice.
Keywords: psychological nursing intervention, family care, radical mastectomy, negative emotions, prognosis effect
1 INTRODUCTION
Breast cancer is a malignant tumor that enormously endangers women, which is known as the three major cancers of the female reproductive system together with cervical cancer and ovarian cancer, with the characteristics of high mortality and high recurrence rate. Breast cancer is generally common among middle-aged and elderly women, especially before and after menopause. However, it recently shows a trend towards younger women due to a variety of factors such as environment, work pressure, lifestyle, and diet[1-3]. The current clinical treatment for breast cancer is tumor resection along with radiotherapy and chemotherapy, and patients bear both physical and mental burden from surgery to chemotherapy. Firstly, surgical treatment not only impacts the secondary sex characteristics that lead to changes in appearance, but also has the possibility of recurrence[4-6]. Secondly, the main purpose of chemotherapy is to eliminate cancer cells. However, patients are susceptible to adverse reactions such as skin diseases, gastrointestinal diseases, hair loss and weight loss, and endocrine disorders after this treatment. Therefore, they inevitably have some negative emotions during treatment, which not only threatens their mental health, but also impacts the prognosis and then prolongs their recovery[7-9]. In order to alleviate their negative emotions in the treatment of patients with breast cancer, psychological nursing intervention is the main nursing method in many hospitals, and also has achieved remarkable results. Family-like care is an auxiliary that gives patients a feeling of familiarity. In this study, patients with breast cancer undergoing radical mastectomy were assigned to receive routine nursing or to receive both psychological nursing interventions and family-like care. The two groups were compared in nursing efficiency, nursing satisfaction, prevalence of adverse reactions, self-rating anxiety scale (SAS) score, self-rating depression scale (SDS) scores, mental status scale in non psychiatric settings (MSSNS) score, Pittsburgh sleep quality index (PSQI) score, quality of life index (QLI) score, and incidence of adverse emotions at 1, 2, 3, and 4 weeks after surgery to analyze the application effect of psychological nursing intervention combined with family-like care in patients with breast cancer.
2 MATERIALS AND METHODS
2.1 General Materials
A retrospective analysis was performed on 100 patients with breast cancer who underwent radical mastectomy in our hospital between September 2018 and September 2020. They were equally allocated to a control group (44 to 56 years old) and an experimental group (45 to 56 years old) according to nursing methods. No statistical significance existed in the comparison of such general materials as age and disease course between the two groups (P>0.05). See Table 1.
Table 1. Comparison of General Materials (x̅ ± s)
Group |
Experimental Group |
Control Group |
t/X2 |
P |
|
Age (years) |
49.96±3.45 |
50.20±3.77 |
0.33 |
0.74 |
|
Height (cm) |
163.19±7.50 |
163.41±7.53 |
0.15 |
0.88 |
|
Weight (kg) |
69.90±8.41 |
69.74±8.55 |
0.09 |
0.93 |
|
Course(months) |
2.43±0.58 |
2.28±0.62 |
1.25 |
0.21 |
|
Clinical types |
I stage (n) |
19 |
20 |
0.04 |
0.84 |
II stage (n) |
15 |
18 |
0.41 |
0.52 |
|
III stage (n) |
16 |
12 |
0.79 |
0.37 |
|
Affected lateral |
Left (n) |
35 |
33 |
0.18 |
0.67 |
Right (n) |
15 |
17 |
|||
Education |
Primary school or under (n) |
4 |
5 |
0.12 |
0.73 |
Middle school (n) |
17 |
15 |
0.18 |
0.67 |
|
High school or above (n) |
29 |
30 |
0.04 |
0.84 |
|
2.2 Inclusion/Exclusion Criteria
2.2.1 Inclusion Criteria
(1) Patients with breast cancer underwent radical mastectomy in line with the clinical manifestations of breast cancer.
(2) Patients aged 18 years old or more.
(3) Patients didn’t suffer any other organic diseases of the heart, lung and kidney.
(4) Patients had no histories of drug allergy and drug abuse, and no bad habits.
(5) The ethics committee of our hospital approved this study, and all participants were willingly involved in the study and signed an informed consent.
2.2.2 Exclusion Criteria
(1) Patients experienced the recurrence of breast cancer.
(2) Patients suffered mental disorder and unable to follow the instructions of this study.
(3) Patients had other malignant tumors.
2.3 Methods
The control group was given routine nursing. In another words, nursing staffs notified patients of the precautions after radical mastectomy, frequently communicated with them, and monitored their diseases in time. If there were prognostic problems, nursing staffs must immediately notify doctors. Furthermore, nursing staffs were well prepared for the possible postoperative complications and reminded patients to take medicines on time according to the prescription. In addition, nursing staffs communicated with family members to improve their awareness of health and solve their confusions.
The experimental group was given psychological nursing intervention and family-like care, mainly from the environmental, cognitive and psychological aspects. Firstly, nursing staffs closely observed the emotion changes, and promptly provided psychological counseling and shared examples with positive energy to eliminate their fear and nerves when they were in bad mood. Secondly, environment is a key factor of impacting their mood. A good and harmonious hospitalization environment significantly offered them better hospitalization experience. Therefore, nursing staffs communicated with inpatients or their families to distract their attentions through the improvement of ward environment, so as to help them have better hospitalization experience. Finally, nursing staffs frequently communicated with families and shared nursing plans to obtain support from them because of their intimacy and long time accompany, so that patients really felt the family-like care.
2.4 Observation Indicators
A comparison was made between the two groups in terms of nursing efficiency, nursing satisfaction, prevalence of adverse reactions, SAS score, SDS score, MSSNS score, PSQI score, QLI score, and incidence of negative emotions at 1, 2, 3, and 4 weeks after surgery.
During nursing, it was considered significantly effective if patients had no adverse reactions and had stable mood. It was considered slightly effective if patients occasionally experienced negative emotions such as silence, irritability and anxiety with relatively short time and few frequencies. It was considered ineffective if patients were often in negative mood that enormously impacted their sleep and daily life.
In this SAS, with 50 points as the boundary, a score of less than 50 indicates ‘normal’; a score of 50-59 indicates mild anxiety; a score of 60-69 indicates moderate anxiety; and a score more than 70 indicates severe anxiety.
In this SDS, with 53 points as the reference score, a score of less than 53 points indicates ‘normal’; a score of 53-62 indicates mild depression; a score of 63-72 indicates moderate depression; and a score of more than 72 indicates severe depression.
In this MSSNS, with 60 points as the boundary, a score of less than 60 points indicates ‘normal’; a score of 60-70 indicates ‘mildly abnormal’; and a score of more than 70 indicates ‘abnormal’[10-12].
QLI comprises the items such as daily activities, work and life, and interpersonal relationships, and the full score for each item is 10. A higher score means better quality of life, and vice versa.
The PSQI score ranges from 0 to 21 scores. A higher score indicates worse sleep quality.
2.5 Statistical Processing
In this study, SPSS20.0 was selected for data analysis, and GraphPad Prism 7 (GraphPad Software, San Diego, USA) for the illustration of data. The measurement data were tested by the t test and analyzed by (mean ± SD), and the counting data were tested by the X2 test and analyzed by [n (%)]. P<0.05 implies a significant difference.
3 RESULTS
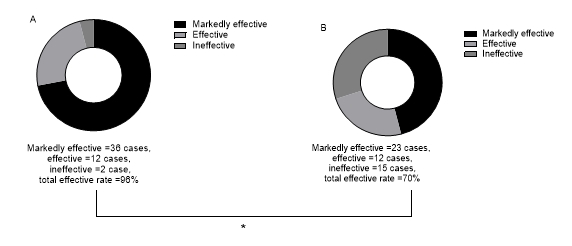
3.1 Comparison of Nursing Efficiency
While comparing nursing efficiency between the two groups, we found that the nursing the experimental group received was more effective than that received by the control group (P<0.05). See Figure 1.
|
Figure 1. Comparison of nursing efficiency. Figure 1A describes the nursing efficiency of the experimental group. Of the cases, 36 cases were markedly effective; 12 cases were effective; and 2 cases were ineffective. The total effective rate was 96%. Figure 1B describes the nursing efficiency in the control group. Of the cases, 23 cases were markedly effective; 12 cases were effective; and 15 cases were ineffective. The total effective rate was 70%. * indicates the comparison of nursing efficiency between the two groups (X2=11.98, P=0.001), and the comparison remains statistically significant.
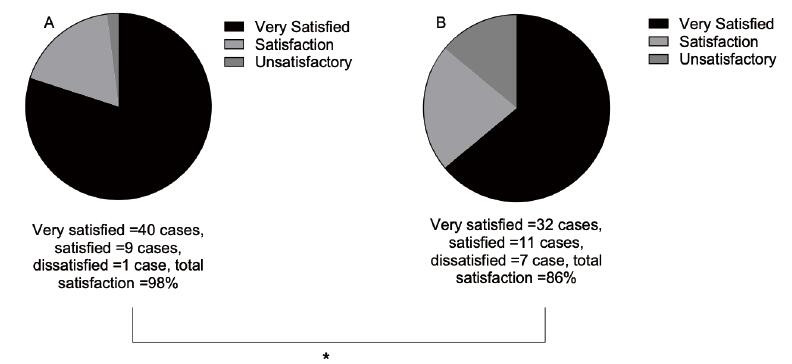
3.2 Comparison of Nursing Satisfaction
The comparison of the nursing satisfaction between the two groups showed that the experimental group was more likely to express higher nursing satisfaction (P<0.05). See Figure 2.
|
Figure 2. Comparison of nursing satisfaction. Figure 2A describes the nursing satisfaction of the experimental group. Of the cases, 40 cases were very satisfied; 9 cases were satisfied; and 1 case was dissatisfied. The total satisfaction rate was 98%; Figure 2B describes the nursing satisfaction of the control group. Of the cases, 32 cases were very satisfied, 11 cases were satisfied, and 7 cases were dissatisfied. The total satisfaction rate was 86%. * means the comparison of nursing satisfaction between the two groups (X2=4.89, P=0.03), and the comparison remains statistically significant.
3.3 Comparison of Prevalence of Adverse Reactions
The comparison of the prevalence of adverse reactions between the two groups during nursing showed that patients the control group were more likely to suffer adverse reactions (P<0.05). See Table 2.
Table 2. Comparison of Prevalence of Adverse Reactions
Group |
Breast Pain |
Surgical Incision Infection |
Fever |
Total Prevalence Rate (%) |
Experimental group |
3 |
0 |
1 |
8% |
Control group |
9 |
3 |
2 |
28% |
X2 |
|
|
|
6.78 |
P |
|
|
|
0.009 |
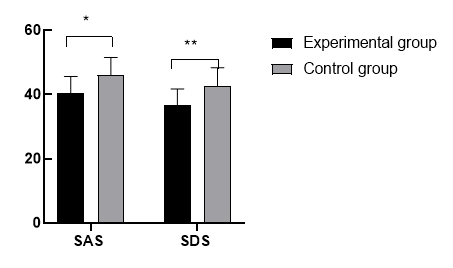
3.4 Comparison of SAS Score and SDS Score
While counting and comparing the SAS and SDS scores of both groups, we found that patients in the experimental group scored lower in SAS and SDS (P<0.05). See Figure 3.
|
Figure 3. Comparison of SAS score and SDS score. The X-axis describes SAS and SDS from left to right, and the Y-axis describes the score. * means the comparison of SAS scores between the two groups [(40.36±5.29) vs. (46.19±5.33), t=5.49, P<0.001]. ** means the comparison of SDS scores between the two groups [(36.68±5.07) vs. (42.73±5.66), t=5.63, P<0.001].
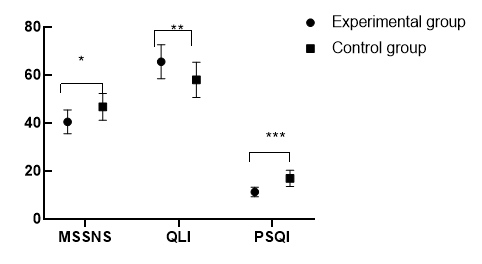
3.5 Comparison of MSSNS Score, PSQI Score, and QLI Score
Both groups performed the MSSNS, PSQI, and QLI tests. The comparison found that patients in the experimental group scored lower in the mental state and sleep quality (both P<0.05), but higher in quality of life (P<0.05). See Figure 4.
|
Figure 4. Comparison of MSSNS score, PSQI score and QLI score. The X-axis describes the MSSNS, QLI and PSQI from left to right, and the Y-axis describes the score. * means the comparison of MSSNS score between the two groups [(40.53±4.99) vs. (46.77±5.62), t=5.87, P<0.001]. ** means the comparison of QLI score between the two groups [(65.58±7.08) vs. (58.02±7.33), t=5.25, P<0.001]. *** means the comparison of PSQI score between the two groups [(11.29±2.00) vs.(16.95±3.37), t=10.21, P<0.001].
3.6 Comparison of Incidence of Negative Emotions at 1, 2, 3, and 4 Weeks After Surgery
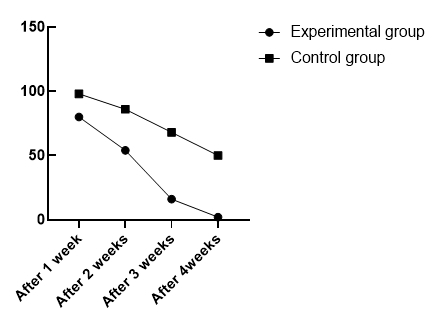
We observed and recorded incidence of adverse emotions at 1, 2, 3, and 4 weeks after radical mastectomy, and then compared them between the two groups. The comparison showed that patients in the control group were more likely to have negative emotions at 1, 2, 3, and 4 weeks after surgery (all P<0.05). See Figure 5.
|
Figure 5. Comparison of incidence of negative emotions at 1, 2, 3, and 4 weeks after surgery. The X-axis describes from left to right after 1 week of nursing, after 2 weeks, after 3 weeks and after 4 weeks. The Y-axis describes the prevalence of negative emotions. The figure describes the comparison of negative emotions between the two groups after 1 week of nursing (80% vs. 98%, X2=8.27, P=0.004), that after 2 weeks of nursing (54% vs. 86%, X2=12.19, P<0.001), that after 3 weeks of nursing (16% vs. 68%, X2=27.75, P<0.001), and that after 4 weeks of nursing(2% vs. 50%, X2=29.94, P<0.001).
4 DISCUSSION
Breast cancer is a malignant tumor in the epithelial tissue of breast, with high fatality and recurrence. Statistics have found that ten thousands of women die of breast cancer, accounting for 7% of malignant tumors, which enormously threatens their health and also heavily impacts the improvement of human health[13-15]. Radical mastectomy is currently the primary treatment for breast cancer, which removes cancer cells by the resection of tumor tissue and prolongs the life. In addition to long-term course, ignorance of the disease progression and inability to accept their own conditions usually put patients into depression during treatment. Negative emotions are harmful and useless, which threatens the physical and mental health of patients, and also compromises the prognosis and recovery[16-18].
Psychological nursing intervention is specifically designed to improve the mental state of patients and alleviate their negative emotions, which has been extensively applied in clinical practice with the update of medical concepts[19-22]. It is reported that family-like care substantially improves the hospitalization experience and the nursing efficiency. In this study, we explored the effect of psychological nursing intervention and family-like care in patients with breast cancer undergoing radical mastectomy. They were given routine nursing and psychological nursing intervention along with family-like care, respectively. Then we compared nursing efficiency, nursing satisfaction, prevalence of adverse reactions, SAS score, SDS score, MSSNS score, PSQI score, QLI score, and incidence of negative emotions at 1, 2, 3 and 4 weeks after surgery.
Our findings indicated that patients in the experimental group scored higher in nursing efficiency, nursing satisfaction, and QLI (all P<0.05), and nursing efficiency was associated with indicators such as prognosis and adverse reactions. Therefore, the findings have revealed that psychological nursing intervention substantially improves the nursing efficiency, prognosis, recovery and quality of life of patients in conjunction with family-like care, and also has been highly recognized by patients and their families, which fully verifies the necessity of its application. Moreover, patients in the experimental group scored lower in the prevalence of adverse reactions, SAS, SDS, MSSNS, and PSQI, and showed a lower incidence of adverse emotions at 1, 2, 3, and 4 weeks than those in the control group (all P<0.05). SAS score, SDS score, and MSSNS score were indicators for the evaluation of mental state and negative emotions. It was seen that psychological nursing interventions dramatically relieved the negative emotions and left patients in good mental state in conjunction with family-like care. The PSQI was used for the evaluation of sleep quality. His/her sleep quality sharply became worse with insomnia and dreaminess, given that a patient had been in negative mood for a long time. Our findings suggested that his/her sleep quality had been improved after nursing intervention. Liu et al.[23] have proposed that family-like care dramatically improves the quality of life after surgery of patients with breast cancer and reduces the prevalence of postoperative complications, similar to our findings, which fully verifies the scientific reliability of our findings.
In summary, psychological nursing intervention combined with family-like care significantly relieves the postoperative negative emotion and improves the prognosis, which has been unanimously recognized by patients. Therefore, this nursing model is of great value in practice.
Acknowledgements
Not applicable.
Conflicts of Interest
The authors declared no conflict of interest.
Author Contribution
All three authors collaboratively designed the study, collected data, analyzed data, and took part in writing the manuscript; all authors approved the final version.
Abbreviation List
MSSNS, Mental status scale in non-psychiatric settings
PSQI, Pittsburgh sleep quality index
QLI, Quality of life index
SAS, Self-rating anxiety scale
SDS, Self-rating depression scale
References
[1] Mughees M, Kumar K, Wajid S. Exosome vesicle as a nano-therapeutic carrier for breast cancer. J Drug Target, 2021; 29: 121-130. DOI: 10.1080/1061186X.2020.1808001.
[2] Ryans K, Perdomo M, Davies CC et al. Rehabilitation interventions for the management of breast cancer–related lymphedema: developing a patient-centered, evidence-based plan of care throughout survivorship. J Cancer Surviv, 2021; 22. DOI: 10.1007/s11764-021-00991-2.
[3] Mastaneh S, Mohsen N, Pouya P et al. Evaluation of sleep disturbance and mood status of breast cancer patients undergoing radiotherapy. Indian J Gynecol Oncol, 2021; 19. DOI: 10.1007/s40944-021-00494-z.
[4] Fadi A, Biljana B, Suzan C et al. Pharmacological activation of pyruvate kinase M2 reprograms glycolysis leading to TXNIP depletion and AMPK activation in breast cancer cells. Cancer Metab, 2021; 9. DOI: 10.1186/s40170-021-00239-8.
[5] Taroeno-Hariadi KW, Hardianti MS, Sinorita H et al. Obesity, leptin, and deregulation of microRNA in lipid metabolisms: their contribution to breast cancer prognosis. Diabetol Metab Syndr, 2021; 13. DOI: 10.1186/s13098-020-00621-4.
[6] Golrokh Mofrad M, Sadigh ZA, Ainechi S et al. Detection of human papillomavirus genotypes, herpes simplex, varicella zoster and cytomegalovirus in breast cancer patients. Virol J, 2021; 18. DOI: 10.1186/s12985-021-01498-z.
[7] Monkkonen T, Traustadóttir GÁ, Koledova Z. Unraveling the breast: advances in mammary biology and cancer methods. J Mammary Gland Biol Neoplasia, 2020; 25: 233-236. DOI: 10.1007/s10911-020-09476-x.
[8] Mondaca JM, Guijarro ACC, Flamini MI et al. Heregulin induced cell migration is prevented by trastuzumab and trastuzumab-emtansine in HER2+ breast cancer. Breast Cancer Res Treat, 2021; 186: 363-377. DOI: 10.1007/s10549-020-06089-0.
[9] Liu H, Yang Y. Effects of a psychological nursing intervention on prevention of anxiety and depression in the postpartum period: a randomized controlled trial. Ann Gen Psychiatry, 2021; 20. DOI: 10.1186/s12991-020-00320-4.
[10] Liu W. The effects of virtual simulation on undergraduate nursing students’ beliefs about prognosis and outcomes for people with mental disorders. Clin Simul Nurs, 2021; 50. DOI: 10.1016/j.ecns.2020.09.007.
[11] Lores T, Goess C, Mikocka-Walus A et al. Integrated psy-chological care reduces health care costs at a hospital-based inflammatory bowel disease service. Clin Gastroenterol Hepatol, 2021; 19. DOI: 10.1016/j.cgh.2020.01.030.
[12] Goh YS, Owyong JQY, Seetoh YM et al. Exploring pedagogies used in undergraduate mental health nursing curriculum: an integrative literature review. Int J Ment Health Nurs, 2021; 30: 47-61. DOI: 10.1111/inm.12816.
[13] Keliat BA, Riasmini NM, Daulima NHC et al. Applying the community mental health nursing model among people with schizophrenia. Enferm Clin (Engl Ed), 2020; 8: S1130-8621(20)30521-0. DOI: 10.1016/j.enfcli.2020.10.024.
[14] Gray R, Thompson DR, Tong Chien W et al. Why has the journal of psychiatric and mental health nursing stopped publishing registered reports? J Psychiatr Ment Health Nurs, 2020; 28: 35. DOI: 10.1111/jpm.12721.
[15] Liao B, Liang M, Ouyang Q et al. Psychological nursing of patients with stroke in China: a systematic review and Meta
analysis. Front Psychiatry, 2021; 11: 569426. DOI: 10.3389/fpsyt.2020.569426.
[16] Zhang H, Wei Q. Research on the status quo of psychological care for AIDS patients in adolescents. J Contemp Educ Res, 2020; 4: 12. DOI: 10.26689/jcer.v4i12.1705.
[17] Zhang X, Bai X, Yan Z. Application of psychological nursing combined with exercise therapy in nursing of gestational diabetes mellitus. Minerva Med, 2020; 27. DOI: 10.23736/S0026-4806.20.07104-9.
[18] Baker C, Rose ML, Ryan B et al. Barriers and facilitators to implementing stepped psychological care for people with aphasia: perspectives of stroke health professionals. Top Stroke Rehabil, 2021; 28: 581-593. DOI: 10.1080/10749357.
2020.1849952.
[19] Ward-Miller S, Farley EM, Espinosa L et al. Psychiatric mental health nursing in the international year of the nurse and COVID-19: One hospital’s perspective on resilience and innovation - past, present and future. Arch Psychiatr Nurs, 2021; 35: 303-310. DOI: 10.1016/j.apnu.2020.11.002.
[20] Liu YT, Chang KY. Study on the effectiveness and cross-functional collaboration of psychiatric nursing for inpatients: an example from a teaching hospital in Taiwan. J Soc Sci Hum, 2020; 2.
[21] Elanie C. Transforming mental health nursing practice with Safewards The Safewards model offers ten interventions to reduce conflict and mental health practitioner Geoff Brennan is the pioneer behind many of these developments. Ment Health Prac, 2020; 23: 10-12. DOI: 10.7748/mhp.23.6.10.s4.
[22] Slade PP, Molyneux DR, Watt DA. A systematic review of clinical effectiveness of psychological interventions to reduce post traumatic stress symptoms following child birth and a meta-synthesis of facilitators and barriers to uptake of psychological care. J Affect Disord, 2021; 281: 678-694. DOI: 10.1016/j.jad.2020.11.092.
[23] Liu J, Huang X, Liu J. Analysis of the effect of cognitive behavior intervention on perioperative nursing of breast can-cer patients. Curr Med, 2019; 25: 183-184.
Copyright © 2021 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.





 Copyright ©
Copyright ©