Analyzation of the Clinical Effects of Fine Nursing Model Combined with Integrated Medical Care Intervention on Elderly Patients with Chronic Obstructive Pulmonary Disease
Xinyun Kang1*, Chuang Dong1, Cuicui Liu1
1 Hebei PetroChina Central Hospital, Hebei Province, China
*Correspondence to: Xinyun Kang, Bachelor, Hebei PetroChina Central Hospital, 51 Xinkai Road, Guangyang District, Langfang city, Hebei 065000, China; Email: 371852122@qq.com
Abstract
Objectives: To study the clinical effects of fine nursing model combined with integrated medical care intervention on elderly patients with chronic obstructive pulmonary disease (COPD), and to further analyze the clinical application value of this nursing model.
Methods: A total of 144 elderly patients who were diagnosed with COPD and received treatments in our hospital from April 2018 to April 2019 were selected as research subjects. The patients were divided into a control group and an experimental group by the random number table method, with 72 cases in each group. The control group adopted routine disease nursing program, while the experimental group adopted intervention program that combined fine nursing and integrated medical care together. Both groups’ pulmonary function related indexes were statistically analyzed after nursing intervention: forced expiratory volume in 1 (FEV1)/forced vital capacity (FVC) (%), 6-minute walking distance (6MWD), modified medical research council (mMRC) dyspnea scales, COPD assessment test (CAT), quality of life (QOL) and nursing satisfaction rate.
Results: The experimental group’s pulmonary function indexes, 6MWD, mMRC dyspnea scales, and CAT scores one month after intervention and half a year after intervention were all significantly better than those of the control group. There were significant differences between two groups (P<0.05). The QOL (physical activity, mentality and social function) and nursing satisfaction rate of the experimental group were significantly higher than those of the control group as well (P<0.05).
Conclusion: The integrated medical care group, which was formed based on the disease development of elderly patients with COPD, was capable of developing customized fine nursing programs according to patients’ individual symptoms. Compared with routine clinical care, this nursing model is more practical. It is good for improving patients’ QOL and their symptoms, raising nursing satisfaction rate, and establishing good doctor-patient relationship. Therefore, it should be widely applied and promoted in clinical practice.
Keywords: fine nursing, integrated medical care, elderly patients with chronic obstructive pulmonary disease (COPD), nursing satisfaction rate
1 INTRODUCTION
The story of human development is a process of fighting against nature and diseases. Along with the development of social civilization and medical level, human’s life expectancy gradually increases, but the problem of aging population and senile diseases’ prevention and treatment have become more and more salient[1,2]. At present, along with the change of human lifestyle, the kind of disease that endangers human health has changes as well. Chronic diseases have become the major threat to human health. Respiratory diseases, cardiovascular diseases, cancers, and diabetes are all common chronic diseases[3]. In recent years, severe environmental pollution in China, including declining air quality and soaring air pollution index, has gradually become the main trigger for respiratory diseases. Patients with chronic respiratory diseases, in particular, are highly sensitive to undesirable air pollutants. Chronic obstructive pulmonary disease (COPD) is a common disease among the elderly. It is chronic bronchitis or emphysema caused by obstructed airflow. Delayed treatment will incur other diseases like pulmonary heart diseases or respiratory failure. The causes are respiratory infections triggered by harmful gas or particle, which further results in inflammation. Patients with COPD need to be hospitalized recurrently, which seriously compromises patients’ physical health and life quality. And it has rather high mortality rate and disability rate[4-6]. Based on previous research, this research is to investigate the clinical effects of effective nursing intervention on elderly patients with COPD and further analyze the clinical value of fine nursing model combined with integrated medical care intervention. The results of this research are discussed as follows.
2 MATERIAL AND METHODS
2.1 General Materials
A total of 144 elderly patients who were diagnosed with COPD and received treatments in our hospital from April 2018 to April 2019 were selected as research subjects. The patients were divided into a control group and an experimental group by the random number table method, with 72 cases in each group. The research objects consisted of 80 male cases and 64 female cases, between 55 to 80 years old, with an average age of (70.1±4.2) years. There were no significant differences in general clinical data and information between the two groups (P>0.05).
2.2 Inclusion Criteria
(1) All the subjects met the diagnostic criteria for COPD listed in Diagnostic criteria for chronic obstructive pulmonary disease (WS318-2010). (2) All the subjects were 55 years old or older. (3) All the subjects had complete and available clinical data. (4) This study had obtained approval from our hospital’s research ethics committee. All the subjects and their family members understood the research’s process and objective, accepted the nursing intervention program, and had signed the informed consent form.
2.3 Exclusion Criteria
(1) Patients with combined lesion of other organ tissues like brain, heart, kidney, and liver; (2) Patients with asthma, elevated eosinophils, or other acute respiratory infections; (3) Patients with cognitive disorder or with poor compliance; (4) Patients with incomplete clinical data.
2.4 Methods
All patients were diagnosed and treated by doctors, and effective COPD treatments were adopted based on patients’ conditions and symptoms. Patients were required to take anti-infectious medicine or anti-inflammatory medicine. Doctors helped patients with expectoration and trachea dilation[7, 8].
For the control group: Routine nursing intervention for COPD was adopted. Medical care staff supervised patients to follow medical instruction according to their treatment method, gave reasonable instruction on patients’ diets, made sure patients avoid poor pathogenic habits, helped patients with respiratory function training regularly, and provided patients with COPD-related health knowledge and effective way of expectoration[9].
For the experimental group: Fine nursing model combined with integrated medical care intervention was adopted. All from the respiratory department, 4 nurses at the same rank and a doctor consisted of the integrated medical care nursing group for pulmonary diseases. The doctor-in-charge was the group leader and managed all the treatment schedules for patients in the experimental group. Group meetings were held every two weeks, all members were required to report patient’s nursing progressing, discuss on related problems, and propose optimized measurements. By establishing a WeChat public account, patients’ condition was timely updated, which was convenient for medical staff to communicate with each other and for patients and their family members to learn their conditions. Before nursing intervention, all group members discussed patients’ conditions and developed customized fine nursing plans. Specific measures including: (1) psychological intervention: COPD is a recurrent disease, which generates negative influence, like dyspnea and poor exercise tolerance, on patients. Many patients are prone to have negative emotions like anxiety, dysphoria and depression. During the nursing process, nurses should be more sensitive to patients’ psychological changes, notice patients’ negative emotions timely, take effective psychological interventions, and help them ease their passive mood [10-13]. (2) Health education: from the beginning of treatment, patients and their family members should be gradually introduced to COPD-related health knowledge, like causes, symptoms, precautions, and emergency treatments. After the nursing intervention has reached certain effects, health lectures should be organized regularly for patients and their family members, COPD-related knowledge should be further popularized. Frequently asked questions should be answered on site, increase elderly patients and their family members’ knowledge on COPD[14,15]. (3) Respiratory function training: resistance respiratory trainer was arranged to instruct patients on respiratory function trainings, including lip contraction respiration, abdominal respiration and controlled respiration, twice a day, which can be adjusted according to patients’ condition[16]. (4) Exercise tolerance training: sports equipment like resistance band, dumbbell and weight-lift were adopted to help patients with activities like body movement, shoulders relaxation and arm circle, increase patients’ exercise tolerance. (5) Expectoration guidance: methods like expectoration equipment and aerosol inhalation were adopted to guide patients to expectorate independently, and relieve their pains[17]. (6) Also, patients were instructed to follow healthy diets, especially balanced nutrition, based on their vital signs and conditions.
2.5 Observation Indexes
2.5.1 Pulmonary Function Related Indexes of the Two Groups
Patients’ pulmonary function related indexes were tested one month after intervention and half a year after intervention, respectively. And forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) (%) was calculated. The differences between the two groups were compared and analyzed.
2.5.2 6-minute walking Distance (6MWD) of the Two Groups
Patients’ 6MWD was tested and calculated one month after intervention and half a year after intervention, respectively. Patients without shortness of breath were required to walk 6 minutes on flat and broad road according to their own physical strength. They could take a short rest if they are lack of strength halfway. Their walking distances within 6 minutes were recorded by nurses.
2.5.3 Modified Medical Research Council (mMRC) Dyspnea Scales of the Two Groups
Patients’ mMRC dyspnea scales were evaluated one month after intervention and half a year after intervention, respectively. There were 5 levels included. Grade 0: Difficulty in breathing only during excessive activity or strenuous activity, which is counted as 4 points; Grade 1: Transient shortness of breath on flat roads or walking uphill, which is counted as 3 points; Grade 2: When walking on flat roads, the speed is slower than that of peers or a break is needed, which is counted as 2 points; Grade3: If you walk on a flat road for a few minutes or about 100 meters, you have shortness of breath and need to stop for a rest, which is counted as 1 point; Grade 4: Difficulty in breathing when putting on or off clothes, which is counted as 0 points.
2.5.4 COPD Assessment Test (CAT) Scores of the Two Groups
Patients were tested before and after nursing intervention, respectively. CAT was used for evaluating patients’ coughing, expectoration, chest congestion, sleeping quality, energy, mood swings, and physical performances. The influences of COPD on patients were observed and documented. It has a total score of 40, and the lower the score, the milder the symptoms.
2.5.5 Life Quality Scores of the Two Groups
Patients’ physical activity, mentality and social function were evaluated with life quality assessment form. The higher the score, the better the patients’ QOL.
2.5.6 Nursing Satisfaction Rate of the Two Groups
Patients’ nursing satisfaction rate was investigated with a hospital-made questionnaire, which included three levels of satisfaction: dissatisfied, moderately satisfied, and very satisfied. It mainly covered the dimensions of nurses’ professional degree, working attitude, working quality, et al. With a total score of 100 points, 90 points and above stands for very satisfied, 70 to 90 stands for moderately satisfied, and70 and below stands for dissatisfied. Overall satisfaction rate=moderately-satisfaction rate + very -satisfaction rate.
2.6 Statistical Analysis
Statistical analysis was performed using the SPSS statistical software 20.0. The enumeration data were examined by 2 and represented by [% (n)]. The measurement data were examined by t test and represented by (x̅ ± s). And P<0.05 was considered as statistically significant.
3 RESULTS
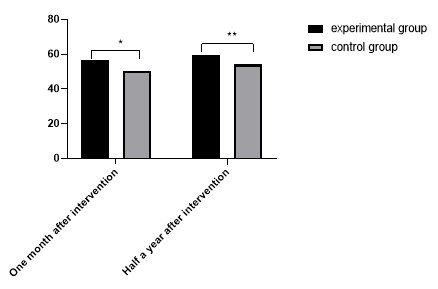
3.1 Comparison of the Two Groups’ Pulmonary Function Related Indexes FEV1/FVC (%)
Patients’ pulmonary function related indexes were tested one month after intervention and half a year after intervention, respectively. And FEV1/FVC (%) was calculated. There were significant differences between two groups’ pulmonary function related indexes. See Figure 1.
Figure 1. Comparison of the Two Groups’ Pulmonary Function (n=72). The horizontal axis stands for timings after intervention, and the vertical axis stands for pulmonary function: FEV1/FVC (%). For the experimental group, the pulmonary function indexes at one month after intervention and half a year after the intervention respectively are (56.8±4.3) and (59.7±4.1), respectively. For the control group, the pulmonary function indexes at one month after intervention and half a year after the intervention respectively are (50.2±4.7) and (54.1±4.3), respectively. The symbol * stands for the significant differences between two groups’ pulmonary function one month after intervention (t=8.7913, P=0.000). The symbol ** stands for the significant differences between two groups’ pulmonary function half a year after intervention (t=7.9977, P=0.000).
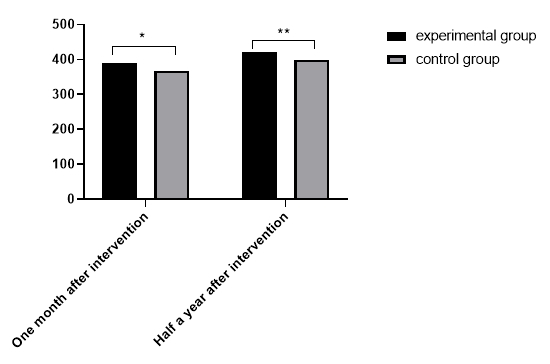
3.2 Comparison of 6MWD between the Two Groups
The 6MWD of patients was tested and calculated one month after intervention and half a year after intervention, respectively. See Figure 2.
|
Figure 2. Comparison of 6-minute walking distance (6MWD) between the two groups (n=72). The horizontal axis stands for timings after intervention, and the vertical axis stands for walking distance (m). For the experimental group, the 6MWD at one month after intervention and half a year after the intervention respectively are (390.1±43.2) m and (421.7±42.6) m, respectively. For the control group, the 6MWD at one month after intervention and half a year after the intervention respectively are (367.4±42.5) and (399.2±43.3) m, respectively. The symbol * stands for the significant differences between two groups’ 6MWD one month after intervention (t=3.1784, P=0.0018). The symbol ** stands for the significant differences between two groups’ 6MWD half a year after intervention (t=3.1431, P=0.002).
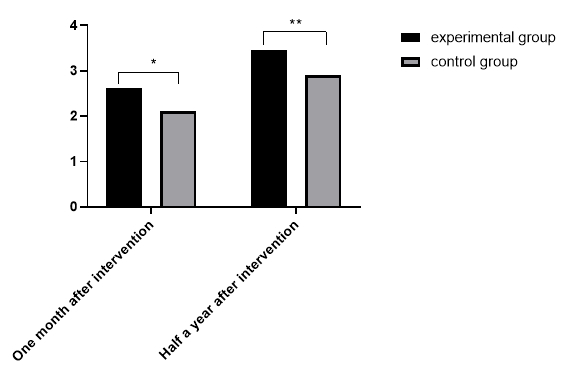
3.3 Comparison of the Two Groups’ Modified Medical Research Council (mMRC) Dyspnea Scores
Patients’ mMRC dyspnea was evaluated one month after intervention and half a year after intervention, respectively. There were significant differences between two groups’ mMRC dyspnea scores. See Figure 3.
|
Figure 3. Comparison of the two groups’ mMRC dyspnea scores (n=72). The horizontal axis stands for timings after intervention, and the vertical axis stands for mMRC dyspnea scores. For the experimental group, the mMRC dyspnea scores at one month after intervention and half a year after the intervention respectively are (2.63±0.83) and (3.46±0.81), respectively. For the control group, the mMRC dyspnea scores at one month after intervention and half a year after the intervention respectively were (2.11±0.82) and(2.91±0.79), respectively. The symbol * stands for the significant differences between two groups’ mMRC dyspnea scales one month after intervention (t=3.7817, P=0.0002). The symbol ** stands for the significant differences between two groups’ mMRC dyspnea scores half a year after intervention (t=4.1247, P=0.0001).
3.4 Comparison of the Two Groups’ COPD Assessment Test (CAT) Scores
From the comparison of both groups’ CAT scores before and after nursing intervention, it could be identified that there were no significant differences between two groups’ CAT scores before nursing intervention (P>0.05). However, after nursing intervention, the experimental group’s CAT scores were significantly lower than those of the control group’s (P<0.001). There were significant differences between two groups’ CAT scores. See Table 1.
Table 1. Comparison of the Two Groups’ COPD Assessment Test (CAT) Scores
Groups |
n |
Before Intervention |
After Intervention |
The experimental group |
72 |
32.1±5.8 |
15.6±5.5 |
The control group |
72 |
31.7±6.1 |
19.8±5.6 |
t |
|
0.4032 |
4.5403 |
P |
|
0.6874 |
<0.001 |
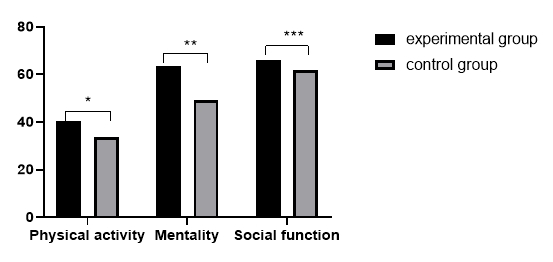
3.5 Comparison of the Two Groups’ Prognosis and Life Quality
Patients’ prognosis and life quality were evaluated. The higher the score, the better the patients’ life quality. See Figure 4.
|
Figure 4. Comparison of the two groups’ prognosis and life quality (n=72). The horizontal axis stands for life quality standards, and the vertical axis stands for life quality scores. For the experimental group, the physical activity score, mentality score and social function score respectively are (40.33±0.96), (63.42±2.16), and (66.07±2.25), respectively. For the control group, the physical activity score, mentality score and social function score respectively are (33.71±1.03), (49.24±2.52), and (61.72±2.21), respectively. The symbol * stands for the significant differences between two groups’ physical activity scores after nursing intervention,(t=39.8947, P=0.000). The symbol ** stands for the significant differences between two groups’ mentality scores after nursing intervention, (t=36.2518, P=0.000). The symbol *** stands for the significant differences between two groups’ social function scores after nursing intervention (t=11.7075, P=0.000).
3.6 Comparison of the Two Groups’ Nursing Satisfaction Rate
Patients’ overall satisfaction rate was investigated with the form of questionnaire. The experimental group’s overall satisfaction rate was significantly higher than that of the control group (P<0.05). There were significant differences between the two groups’ satisfaction rate. See Table 2.
Table 2. Comparison of the Two Groups’ Nursing Satisfaction Rate (n=72)
Groups |
Dissatisfied |
Moderately Satisfied |
Very Satisfied |
Overall Satisfaction Rate |
The experimental group |
2.78% (2/72) |
15.28% (11/72) |
81.94% (59/72) |
97.22% (70/72) |
The control group |
1.25% (9/72) |
27.78% (20/72) |
59.72% (43/72) |
87.5% (63/72) |
X2 |
|
|
|
4.8230 |
P |
|
|
|
0.028 |
4 CONCLUSION
Nowadays, COPD has gradually becoming a threat to human health. It has become a worldwide public health issue, especially for the elder due to their decreased metabolic ability and body function. Also, many elderly patients suffer a lot both physically and mentally because of the recurrent nature of COPD. Therefore, developing effective nursing programs in clinical treatments has become the key to cure this disease. Through integrated medical care groups and customized fine nursing program, elderly patients with COPD can be cured with less time invested[18,19].
This study selected a total of 144 elderly patients who were diagnosed with COPD and received treatments in our hospital from April 2018 to April 2019 as research subjects. And the results showed that the experimental group’s pulmonary function indexes, 6MWD, mMRC dyspnea scales, and CAT scores one month after intervention and half a year after intervention were all significantly better than those of the control group (P<0.05). This proved that the experimental group had better prognosis recovery effects. Under the integrated group’s fine nursing intervention, patients’ condition was better controlled, and their body functions were restored well. The experimental group’s QOL (physical activity, mentality, and social function) was significantly higher than that of the control group as well (P<0.05). This illustrated that patients in the experimental group not only were effectively cured, but also had their physical function restored with less time invested, which improved their prognosis QOL. Also, the experimental group’s nursing satisfaction rate was significantly higher than that of the control group (P<0.05). This further proves that fine nursing model improves patients nursing satisfaction rate, which is beneficial for building a harmonious doctor-patient relationship. The result of our research is in accordance with Shweta et al.’s research[20], which suggests that “the integrated medical care model provides COPD curative effects with effective guarantee, and it effectively increases patients’ treatment compliance, enhances patients’ trust in medical care personnel, and improves patients’ prognosis quality of live”.
In conclusion, for elderly patients with COPD establishing integrated medical care groups and developing customized fine nursing program based on their individual symptoms can effectively improve their QOL and body function. This nursing model has significant clinical application value and should be widely applied and promoted.
Acknowledgements
Not applicable.
Conflicts of Interest
These authors declared no conflict of interest.
Author Contribution
All authors collaboratively designed the study, collected data, analyzed data, and took part in writing the manuscript; all authors approved the final version.
Abbreviation List
CAT, COPD assessment test
COPD, Chronic obstructive pulmonary disease
FEV1, Forced expiratory volume in 1second
FVC, Forced vital capacity
mMRC, Modified medical research council
QOL, Quality of life
6MWD, Six-minute walking distance
References
[1] Totaro M, De Vita E, Giorgi S et al. Comparison of anolyte and chlorine dioxide for a continuous hot water disinfection in nursing home: a two-year legionnaires' disease prevention. J Water Resour Prot, 2019; 11: 233-243. DOI: 10.4236/jwarp.2019.113014.
[2] Pierce DM, Gugliucci MR, Weaver SA. Functional contentment model: optimizing quality of life for nursing home residents with dementia. Int J Clin Exp Med, 2019; 10: 439-451. DOI: 10.4236/ijcm.2019.109037.
[3] Pontin D, Thomas M, Jones G et al. Developing a family resilience assessment tool for health visiting/public health nursing practice using virtual commissioning, high-fidelity simulation, and focus groups. J Child Health Care, 2020; 24: 195-206. DOI: 10.1177/1367493519864743.
[4] Hendriks RA, de Jong PGM, Admiraal WF et al. Instructional design quality in medical massive open online courses for integration into campus education. Med Teach, 2020; 42: 156-163. DOI: 10.1080/0142159X.2019.1665634.
[5] Liao XJ, Li Y, Qian L et al. Research on the application of WeChat supported PBL in English teaching of basic chemistry for higher medical education for international medical students. Creative Educ, 2020; 11: 1690-1696. DOI: 10.4236/ce.2020.119123.
[6] Wang X, Yuan H. Confrontation and integration: the present and future of forensic examinations on medical damage in China. J Forensic Sci Med, 2019; 5: 204-207.
[7] Lu H, Xu DC, Yang YX et al. Genetic polymorphisms of CYP2C9/CYP2C19 in chronic obstructive pulmonary disease. COPD, 2020; 17: 595-600. DOI: 10.1080/15412555.2020.1780577.
[8] Alsharaway LA. Pulmonary rehabilitation outcome in chronic obstructive pulmonary disease patients with a different body composition. Egypt J Bronchology, 2019; 13: 616-622. DOI: 10.4103/ejb.ejb_33_19.
[9] Qin JQ, Deng XL, Wei AQ et al. Correlation between hypocalcemia and acute exacerbation of chronic obstructive pulmonary disease in the elderly. Postgrad Med, 2019; 131: 319-323. DOI: 10.1080/00325481.2019.1585689.
[10] Garb AAM, Abd El Raoof MES, Abd-Elhamed SS et al. Risk factors of cognitive dysfunction among patients with chronic obstructive pulmonary disease. Egypt J Psychiat, 2020; 41: 33-40. DOI: 10.4103/ejpsy.ejpsy_37_19.
[11] Wang P, Zhu M, Zhang D et al. The relationship between chronic obstructive pulmonary disease and non-small cell lung cancer in the elderly. Cancer Med, 2019; 8: 4124-4134. DOI: 10.1002/cam4.2333.
[12] Hirai K, Tanaka A, Homma T et al. Comparison of three frailty models and a sarcopenia model in elderly patients with chronic obstructive pulmonary disease. Geriatr Gerontol Int, 2019; 19: 896-901. DOI: 10.1111/ggi.13740.
[13] Kim T, Choi H, Kim J. Association between dietary nutrient intake and chronic obstructive pulmonary disease severity: a nationwide population-based representative sample. COPD, 2020; 17: 49-58. DOI: 10.1080/15412555.2019.1698530.
[14] Beghé B, Fabbri LM, Garofalo M et al. Three-year hospita-lization and mortality in elderly smokers with chronic obstructive pulmonary disease or chronic heart failure. Respiration: Int Rev Thorac Dis, 2019; 97: 223-233. DOI: 10.1159/000492286.
[15] Cha YH, Ha YC, Park HJ et al. Relationship of chronic obstructive pulmonary disease severity with early and late mortality in elderly patients with hip fracture. Injury, 2019; 50: 1529-1533. DOI: 10.1016/j.injury.2019.05.021.
[16] Luan GJ, Yin P, Wang LJ et al. Association between ambient temperature and chronic obstructive pulmonary disease: a population-based study of the years of life lost. Int J Environ Health R, 2019; 29: 246-254. DOI: 10.1080/09603123.2018.1533533.
[17] Guerriero M, Caminati M, Viegi G et al. Prevalence and features of asthma–chronic obstructive pulmonary disease overlaps in Northern Italy general population. J Asthma, 2019; 56: 27-33. DOI: 10.1080/02770903.2018.1424190.
[18] Feng HR, Zhang C, Ying SM. Classical and emerging therapies against chronic obstructive pulmonary disease. Chin Med J (Engl), 2018; 131: 1894-1897. DOI: 10.4103/0366-6999.238133.
[19] Aggarwal AN. Inhaled corticosteroids in chronic obstructive pulmonary disease: moving toward precision medicine. Int J Noncommunicable Dis, 2019; 4: 1-3. DOI: 10.4103/jncd.jncd_15_19.
[20] Kukrety SP, Parekh JD, Bailey KL. Chronic obstructive pulmonary disease and the hallmarks of aging. Lung India, 2018; 35: 321-327. DOI: 10.4103/lungindia.lungindia_266_17.
Copyright © 2021 The Author(s). This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.




 Copyright ©
Copyright ©