Air Embolism During Prone Position Spine Surgery
Tao Shi1*, Xuewu Xing2, Yiwei Shi3, Wenguang Pang3, Gang Wang3
1Department of Orthopedics, Shenzhen Qianhai Taikang Hospital, Shenzhen, Guangdong Province, China
2Department of Orthopedics, Tianjin First Central Hospital, School of Medicine, Nankai University, Tianjin, China
3Department of Anesthesia, Tianjin First Central Hospital, School of Medicine, Nankai University, Tianjin, China
*Correspondence to: Tao Shi, MD, Chief Technician, Department of Orthopedics, Shenzhen Qianhai Taikang Hospital, No. 3099, Menghai Avenue, Nanshan District, Shenzhen, 518000, Guangdong Province, China. E-mail: shitaostone@163.com
DOI: 10.53964/cme.2025003
Abstract
Venous air embolism (VAE)-induced intraoperative cardiac arrest (CA) is an uncommon but dangerously surgical complication. The study’s objective was to provide an overview of the causes, management, and avoidance of CA brought on by VAE. Combining with a case, and literature reviewing analyzed CA caused by VAE. There have been some case reports about the occurrence of VAE during spine surgery in the prone position, especially in scoliosis and fusion operations. Two weeks following surgery, the patient was released from the hospital without any issues. In addition to this instance, there were 19 more occurrences of VAE linked to prone spine surgery. Ten of the 19 patients passed away, meaning the mortality rate was 52.63%. A gradient greater than 5cm between the right heart and the top pole of the incision can be caused by low blood volume, low central venous pressure, and surgery performed in the sitting or prone posture. VAE requires the open cancellous bone surfaces and valve-less venous plexus of Batson. VAE is a very serious but rare complication of spine surgery and occurs at any time during the operation. Spine surgeons should pay attention to the fatal results caused by VAE and prevent its occurrence.
Keywords: spine surgery, venous air embolism, cardiac arrest, prone position, trauma
1 INTROCUCTION
An extremely uncommon side effect of spine surgery is cardiac arrest (CA). While the frequency of CA in spine surgery is unclear, it is estimated to be 0.7% in heart surgery[1]. For every 1000 lumbar spine surgical operations, there were 6.7 cases of cardiac problems[2]. Venous air embolism (VAE) is more prevalent than in spine operations and is more common following cranial procedures and/or seated surgery[3,4]. Few reports of CA brought on by VAE following spine surgery exist[5-8]. Additionally, reports on the incidence of gas embolism during spine surgery have been made[9,10]. The problems brought on by gas embolism in patients undergoing spine surgery were extensively detailed in those case studies.
We report a case of CA due to VAE that happened during thoracolumbar inter-body fusion and posterior decompression of the spinal canal for a burst fracture of T11, dislocation of T10/T11, and bilateral locked facet of T10/T11 while the patient was prone. Reminding spine surgeons of the possibility of VAE when doing posterior spine surgery in the prone position is the goal. The intention is for spine surgeons to be aware of the potential for these issues in order to develop treatment strategies and preventative measures that will lower the morbidity and death rate in cases that are similar to one another.
2 CASE PRESENTATION
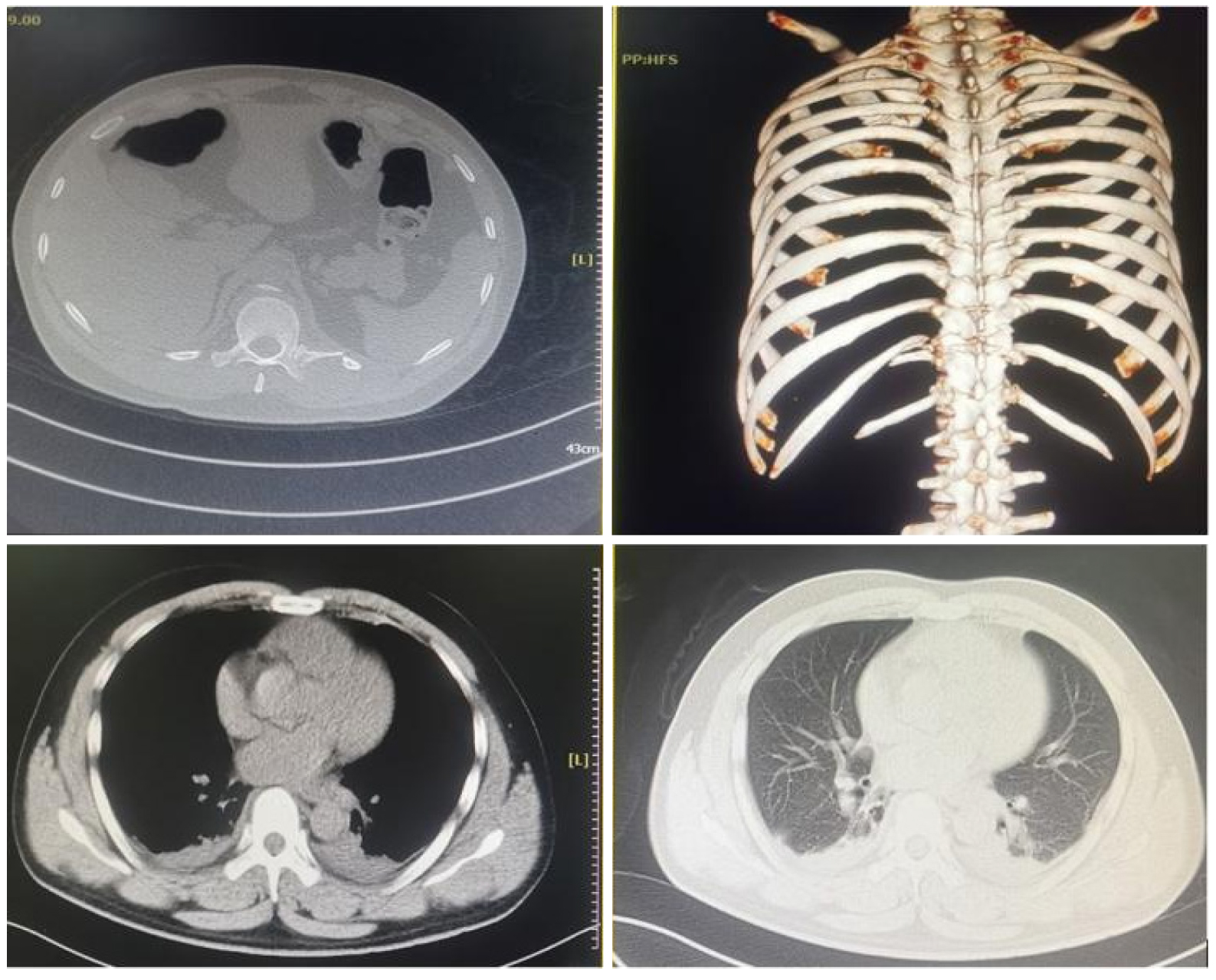
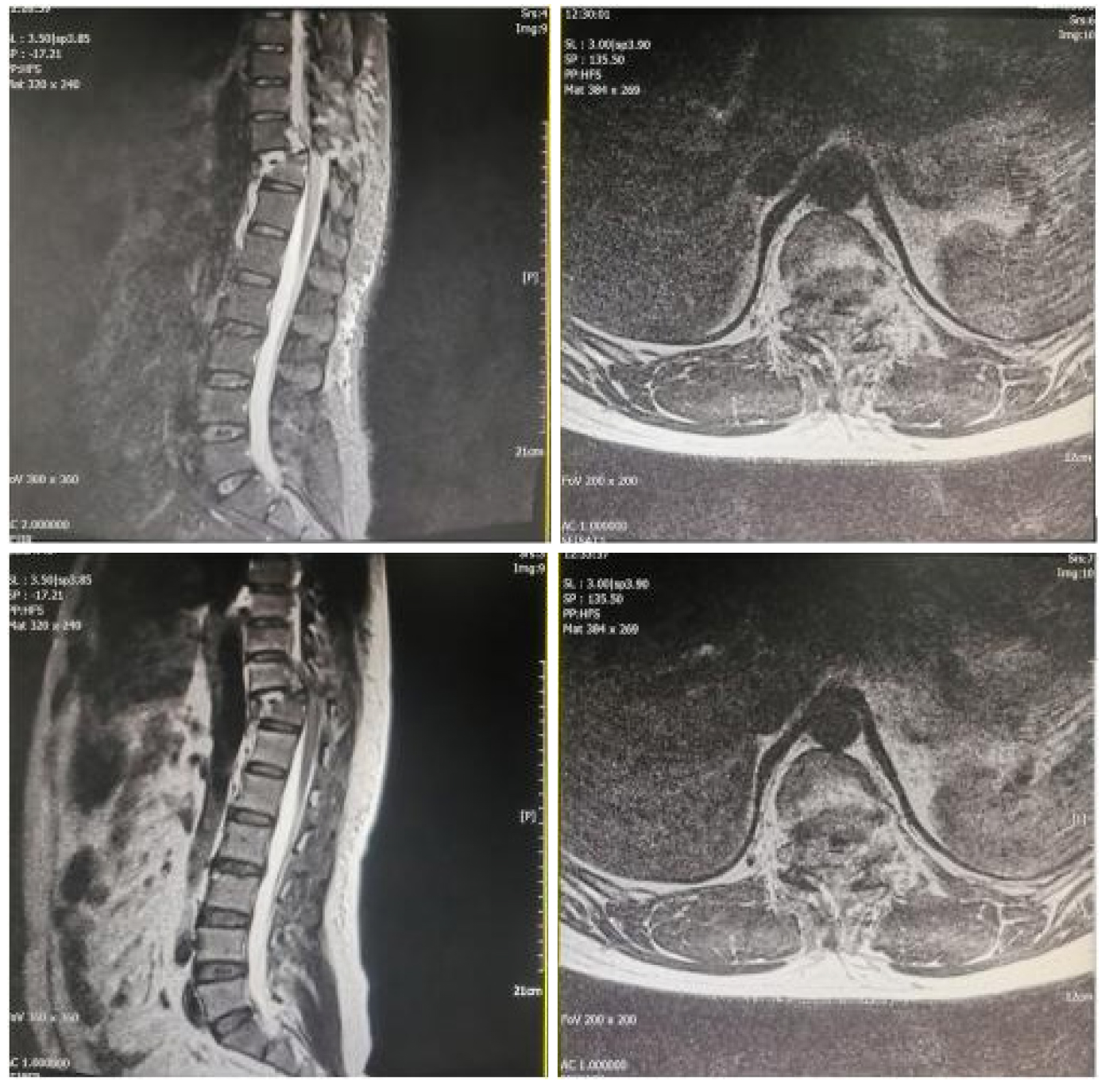
A 37-year-old man working as a construction worker, weighing 80kg and standing 175cm tall, with two children, East Asian ancestry, Han nationality, and no alcohol or tobacco use, unintentionally fell from a height of four meters while at work. During the fall, his thoracolumbar area made contact with a hard surface. Following landing, the patient had back discomfort, neither lower extremity sensation nor movement, but both upper extremities were feeling and moving normally. Within twenty-four hours of the spine trauma, he was admitted to the hospital. The injuries to the spine and chest were evaluated using magnetic resonance imaging (MRI) and computed tomography (CT) images. The images revealed a posterior rib fracture at T11 with dislocation (Figure 1), a posterior rib fracture at T11 with dislocation (Figure 1), a burst fracture of T11 (Figure 2), bilateral locked facet of T10/T11 (Figure 2) and injuries to the spinal cord and posterior ligamentous complex (PLC) (Figure 3). According to the American Spinal Injury Association’s (ASIA) classification, spinal cord function was Grade A. The standard preoperative hematology test came back normal. Both the lower extremity ultrasounds and the echocardiogram came back normal. ASIA Grade A nerve function was present.
|
Figure 1. T11 Posterior Rib Fracture with Dislocation and Mild Pleural Effusion.
|
Figure 2. T11 Burst Fracture and Dislocation of T10/T11 and Bilateral Locked Facet of T10/T11.
|
Figure 3. Injuries of Spine Cord and Posterior Ligamentous Complex PLC.
The patient was given antibiotic prophylaxis with cefuroxime sodium 1,000mg prior to surgery. Tracheal intubation was used to induce anesthesia for the procedure, and propofol and sufentanil were used to keep the patient unconscious. To track arterial blood pressure, the unilateral radial artery was catheterized. Pedicle screws were placed at the pedicle of the vertebral arch at T9, T10, T12, and L1. Both the bilateral superior and inferior articular processes of T11, the spinous process, the bilateral vertebral plate, the interspinous ligaments, the supraspinous ligament, and the ligamentum flavum of T10/T11 and T11/T12 were removed. The T10/T11 vertebral body dislocation was fixed. The spinal canal's bone pieces were extracted. The intervertebral disc of T10/T11 was removed. For the purpose of bone grafting, the T10 inferior end plate and the T11 superior end plate were prepared. Granules (<2mm) were removed from the spinous process, bilateral vertebral plate, and bilateral superior and inferior articular processes of T11. The titanium mesh and bone fragments were introduced into the T10/T11 interverbral space. The transverse connecting rod, lock nuts, and titanium rod were put in place. After saline washing, the wound was sutured. There were 270min in the operation. There was a 1,000ml blood loss and an 800ml transfusion volume.
During the skin suturing procedure, the patient had tachycardia, hypotension, fast oxygen desaturation, and bradycardia all at once after half of the subcutaneous soft tissue had been sutured. His blood pressure was 60/40mmHg, his heart rate was 50 beats per minute, and his oxygen saturation (SpO) was 98%. CA happened when the radial artery’s arterial blood pressure and the blood pressure measured by the cuff were unexpectedly absent from the display. From tachycardia to CA, the entire process took around one minute.
An intravenous injection of 1mg of epinephrine was given when CA developed. The heart rate restored to 140 beats per minute following the injection. His measurements were 120/80mmHg. 100% of the oxygen was saturated (SpO2). Nevertheless, it was impossible to keep the patient’s blood pressure within normal bounds. An instant central venous catheterization was carried out. Using a micro-pump, 7mL/h of norepinephrine was delivered. After that, the skin was fully sutured.
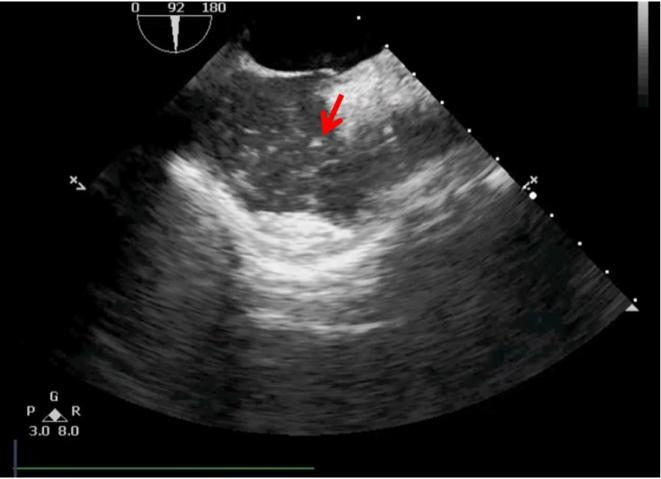
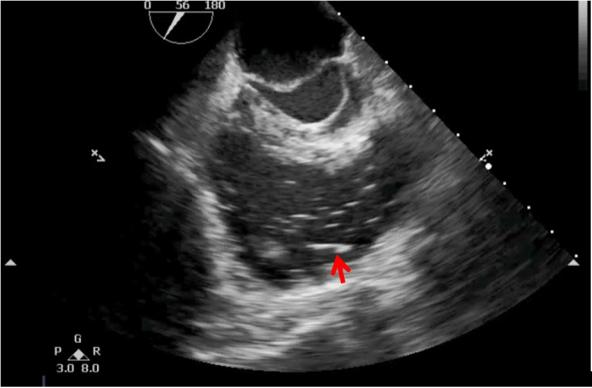
The sick person was placed on the bed. Right away, trans-esophageal echocardiography was performed. The right atrium (Figure 4) and right ventricle (Figure 5) both showed several little bubbles. The tiny bubbles were consistently observed by trans-esophageal echocardiography; however, after half an hour, they vanished from the right ventricle.
|
Figure 4. The lots of Little Bubbles Displayed in the Right Atrium.
|
Figure 5. The lots of Little Bubbles Displayed in the Right Ventricle.
After being put under anesthesia, the patient was sent to the recovery room. Dobutamine 10mL/h and norepinephrine 5mL/h were given by micro-pump. It took the patient sixtymin to come out of anesthesia and into the recovery room. His blood pressure was about 120/75mmHg, his heart rate was about 100 beats per minute, and his oxygen saturation SpO2 was 100%. The endotracheal tube was then taken out. The patient conversed with the physicians and nurses while aware. Albumin supplements and fluid infusion were maintained. The blood test results and the vital signs, which were constantly monitored until they could no longer be read 24h following surgery, were used to gradually reduce the dosage of vasopressors. 48h following surgery, a computed tomography pulmonary angiography (CTPA) was conducted. The CTPA results were normal, and there were no signs of pulmonary embolism.
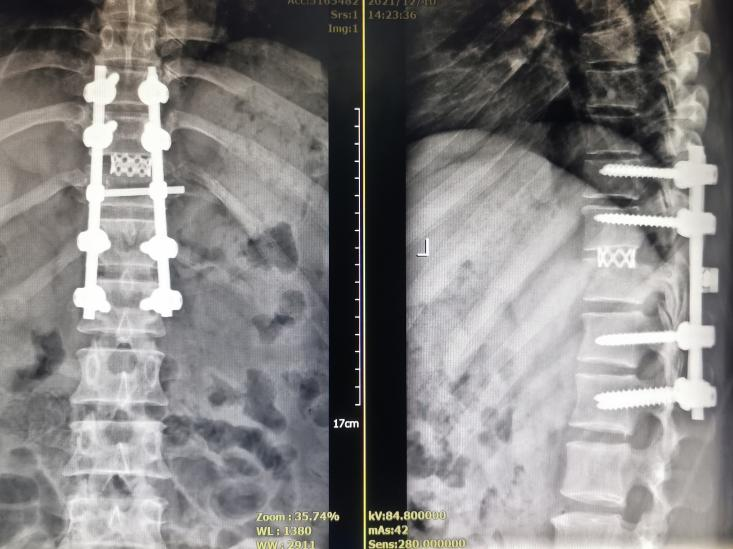
Two weeks following surgery, the patient was released. The categorization of the ASIA still indicated that the spinal cord function was Grade A. The patient's thoracolumbar brace allowed them to sit. The cut has closed up. A little amount of pleural effusion was seen in the left thoracic cavity. The organs showed no signs of embolism. Table 1 displayed the results of blood test before and after CA. Figure 6 showed the X-ray after surgery.
Table 1. Blood Tests Before Operation, Intra-Operation and Before, During and After Complication
Measurement |
Before Operation |
Intra-Operation |
Before Complication |
During Complication |
2h After Complication |
2 Weeks After Complication |
RBC (109/L) |
5.53 |
- |
- |
- |
3.35 |
4.31 |
HGB (g/L) |
160 |
95 |
147 |
162 |
75 |
131 |
WBC (109/L) |
10.98 |
- |
- |
- |
29.98 |
6.27 |
HCT (%) |
47.2 |
29.3 |
45.2 |
49.6 |
23 |
40.40 |
ALB (g/L) |
41.3 |
- |
- |
- |
10.7 |
48.2 |
Sodium (mmol/L) |
138.8 |
139 |
140 |
137 |
137 |
137.7 |
Potassium (mmol/L) |
4.35 |
3.9 |
4.2 |
5.8 |
4.0 |
4.32 |
Chloride (mmol/L) |
99.6 |
109 |
117 |
118 |
107 |
98.5 |
Urea (mmol/L) |
255.4 |
- |
- |
- |
10.67 |
7.04 |
Crea (mmol/L) |
76 |
- |
- |
- |
79 |
58 |
PH |
7.42 |
7.36 |
7.35 |
7.17 |
7.51 |
7.396 |
PO2 (mmHg) |
82 |
93.3 |
91.4 |
82.6 |
149 |
110.3 |
PCO2 (mmHg) |
32.2 |
32.3 |
34.5 |
40.7 |
26.9 |
35.8 |
Glucose (mmol/L) |
8.89 |
9.4 |
8.6 |
10.8 |
7.5 |
4.48 |
Lac (mmol/L) |
- |
0.8 |
1.1 |
5.3 |
0.8 |
3.9 |
Troponin T (pg/mL) |
- |
- |
- |
- |
60.7 |
6.2 |
|
Figure 6. X-ray After Surgery.
3 DISCUSSION
Table 2. Cases of Ca Caused by Vae Associated Spine Surgery in the Prone Position from Literatures
References |
Age/Sex |
Diagnosis |
Surgery |
Level |
Outcome |
Lang et al.[11], 1989 |
16/M |
Duchenne muscular dystrophy |
Fusion |
- |
Died |
McCarthy et al.[12], 1990 |
18/F |
Idiopathic scoliosis |
Fusion |
- |
Died |
McCarthy et al.[12], 1990 |
15/M |
Congenital scoliosis |
Fusion |
- |
Died |
Albin et al.[13], 1991 |
55/M |
Lumbar disc herniation |
Fusion |
L4/L5 |
Survived |
Albin et al.[13], 1991 |
40/M |
Lumbar disc herniation |
Fusion |
L3/L4 |
Died |
Albin et al.[13], 1991 |
40/M |
Lumbar disc herniation |
Fusion |
L5/S1 |
Died |
Horlocker et al.[14], 1992 |
NR |
- |
Spinal instrumentation |
- |
Died |
Horlocker et al.[14], 1992 |
NR |
- |
Spinal instrumentation |
- |
Survived |
Sutherland et al.[15], 1997 |
8/F |
Idiopathic scoliosis |
Fusion |
T1-S1 |
Died |
Sutherland et al.[15], 1997 |
12/F |
Idiopathic scoliosis |
Fusion |
T2-S1 |
Died |
Pham Dang et al.[16], 2002 |
46/F |
Degenerative scoliosis |
Fusion |
T10-L3 |
Survived |
Wills et al.[17], 2005 |
14/F |
Idiopathic scoliosis |
Fusion |
T3-L4 |
Survived |
Wills et al.[17], 2005 |
13/F |
Idiopathic scoliosis |
Fusion |
T3-L1 |
Died |
McDouall et al.[18], 2007 |
43/F |
Lumbar spinal stenosis |
Laminectomy |
L4/L5 |
Died |
Dumont et al.[19], 2010 |
38/M |
Atlantoaxial instability |
Fusion |
C1-C2 |
Survived |
Cruz et al.[20], 2016 |
65/M |
Nonunion of dens fracture |
Fusion |
C1/C2 |
Survived |
Lee-Archer et al.[21], 2017 |
10/F |
Kyphoscoliosis |
Fusion |
C5/L4 |
Survived |
Naohisa Miyakoshi et al.[7], 2019 |
41/M |
OPLL and OLF |
Laminectomy |
C2-T4 |
Survived |
Present case |
37/M |
Spine fracture and dislocation |
Fusion |
T10/T11 |
Survived |
As shown in Table 2, CA mostly occurred during deformity or spine fusion procedures. During spine surgery in the prone position, VAE unlikely to occur due to the lack of virtually any gravitational gradient between the surgical wound and the right ventricle, as well as the high central venous pressure caused by being in the prone position. But there were other risks of VAE: 1) Major surgery and long operation time: major surgery always requires a larger incision and wound, thereby leaving a larger wound, and extensive exposure of cancellous bone surfaces, thereby resulting in a long operation time, and a higher potential for air to enter the vein through the open cancellous bone surfaces. To avoid the above situation, the open cancellous bone surfaces should be sealed with bone wax in a timely manner. 2) Incomplete hemostasis: bleeding of the venous plexus of the spine canal during spine surgery sometime is sometimes serious, and if hemostasis is achieved in a timely manner, air can enter vein through Batson’s valve-less venous plexus. 3) an incompletely closed wound. Operative procedures sometimes need to be at the local site during the surgery. At this time, the non-operative site of the wound should be stuffed with gauze to avoid contact with air; if not, air may enter the vein through the wound.
Basic life support must be initiated right once if CA is suspected and later confirmed during the procedure. An expert critical care specialist or anesthesiologist is needed for the rescue procedure. Currently, spine surgeons are crucial in cases involving the safe rotation of patients from the prone position. The patient should be put in the supine position as soon as feasible if they require cardio-pulmonary resuscitation (CPR). Tamponade, sterile covering and temporary closure are necessary for the wound. In our instance, the anomalous state in the central anesthesia control room was recognized by a senior anesthesiologist who came. To carry out the rescue treatment, two seasoned anesthesiologists collaborated with the nurses and senior anesthesiologist. In addition CA occurred at the end of skin suturing, not during the operation, which facilitated the rescue. During the rescue procedure, CA was temporary.
According to previous studies, there are several reasons for VAE occurrence. The first is the patent foramen ovale (PFO) and the operative position such as the sitting or semi-seated position. This phenomenon mainly occurred in neurosurgery. Air embolism can result in paradoxical embolism with an infarction in the heart or brain through the right-to-left shunt. However a study showed that air embolism occurred in 33 of these 82 patients (40.2%), and in 4 studies no paradoxical embolisms were detected in neurosurgical patients with PFO who underwent the procedure in the semi-sitting position[26]. In this case, a PFO was not detected by echocardiography.
The second is the use of hydrogen peroxide (H2O2) solution for irrigating wounds. There have been some reports about the occurrence of oxygen embolism after the use of H2O2 solution for wounds irrigations during spine surgery[9,10]. There are several potential mechanisms for this phenomenon, including: 1) High-pressure oxygen created by H2O2 being drawn into a ruptured dural sac or damaged inter-muscular vein, which over time forms an air embolus[27-30]; 2) Oxygen bubbles may be absorbed more quickly by vascular-rich cancellous bone when under pressure; 3) H2O2 may pass through endothelial cells via water channels (aquaporins) in the cell membranes, which could explain how an intact tissue can have a gas embolus[31]; and 4) Excessive H2O2 can produce peroxynitrite, which endothelial cells cannot quickly process, leading to intimal rupture and a subsequent gas embolism[32]. Here, irrigation of surgical incisions with H2O2 was never done.
The third is the presence of visible air bubbling at the operation site, thereby leading to VAE. The air bubbling at the operating site signaled the commencement of cardiovascular collapse owing to a major VAE in the current instance. Wills et al.[17] hypothesized an air bubbling mechanism in conjunction with a huge VAE. Air can enter the venous system through open cancellous bone surfaces or Batson's valve-less venous plexus due to a hydrostatic gradient[15,33]. The air then passes through the right side of the heart to reach the pulmonary arterial arteries. It is possible to develop an intra-cardiac “airlock”, which renders the heart pump inefficient and obstructs forward flow[17]. This “airlock” results in an increase in central venous pressure, which drives retrograde flow through the valveless venous system and pushes entrained air out of the venous system[17]. Furthermore, variations in intra-thoracic pressure caused by ventilation can cause air to be pulled into the venous circulation, followed by retrograde blood and air flow out of the exposed veins[17]. In this case there was no visible air bubbling at the operation site, but there was a hydrostatic gradient. This may be the reason for CA caused by VAE in our case report.
3.1 Mechanism of CA caused by VAE
Apart from the aforementioned circumstance, the paravertebral venous system also contributes to the process of air entering veins. The paravertebral venous system is described by Batson as paralleling and communicating with the superior and inferior vena cavae. The dural sinuses serve as the cranial endpoint for the vein plexus, which runs the whole length of the vertebral column[34]. Additionally, he mentioned that air that enters the vertebral vein system might go to the skull and block the cerebral veins. When the interosseous intravascular pressure drops during inspiration, Moe and Winter have observed that air may enter through exposed decorticated bone on the open cancellous bone surfaces[35].
VAE can arise as a result of many variables, including the patient's posture and the surgical site. Compared to back or stomach surgery, head and neck surgery had a greater incidence of air embolism[36]. Furthermore, there is a correlation between the rate of embolization and the volume of air embolized and morbidity and death[37-39]. A modest amount of air injected slowly might not have any effects, but a high volume injected quickly 3-8cc/kg might block the pulmonary outflow tract and be dangerous[40]. Holt discovered that dogs could not survive 3cc/kg of air[41]. In a 70kg person, this translates to 210cc.
3.2 Pathological changes caused by VAE
A portion of the air that travels to the pulmonary artery's terminal branches has the potential to seriously damage lung tissue and induce acute pulmonary edema. Animals with these terminal branches have also been reported to have fibrin plugs[39,42]. Postoperative technetium pertechnetate macroaggregates with albumin and lung scans show that air embolism causes perfusion deficits that are proportionate in size to the volume of air aspirated, according to a study of patients who had survived intraoperative pulmonary air embolism[39].
4 CONCLUSION
VAE is a very serious but rare complication of spine surgery that occurs at any time during the operation. Spine surgeons should be aware of the fatal results caused by VAE and work to prevent its occurrence.
Acknowledgments
The authors acknowledge all of the doctors and anesthetists who contributed to rescue the patient.
Informed Consent Statement
Written informed consent was obtained from the patient for publication of this report and all accompanying images.
Conflicts of Interest
The authors declared no conflict of interest.
Data Availability
All data generated or analyzed during this study are included in this published article.
Copyright Permission
Copyright © 2025 The Author(s). Published by Innovation Forever Publishing Group Limited. This open-access article is licensed under a Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits unrestricted use, sharing, adaptation, distribution, and reproduction in any medium, provided the original work is properly cited.
Author Contribution
Xing X, Shi Y, Pang W, and Wang G collected the data, while Shi T and Xing X analyzed it. Shi T wrote the paper, and Xing X and Shi Y interpreted the results. All authors have read and approved the final manuscript.
Abbreviation List
ASIA, American Spinal Injury Association
CA, Cardiac arrest
CPR, Cardio-pulmonary resuscitation
CT, Computed tomography
CTPA, Computed tomography pulmonary angiography
MRI, Magnetic resonance imaging
PFO, Patent foramen ovale
PLC, Posterior ligamentous complex
SpO, Oxygen saturation
VAE, Venous air embolism
References
[1] Anthi A, Tzelepis G E, Alivizatos P et al. Unexpected cardiac arrest after cardiac surgery: incidence, predisposing causes, and outcome of open chest cardiopulmonary resuscitation. Chest, 1998; 113: 15-19.[DOI]
[2] Fineberg S J, Ahmadinia K, Patel AA et al. Incidence and mortality of cardiac events in lumbar spine surgery. Spine, 2013; 38: 1422-1429.[DOI]
[3] Ballantine RI. Anaesthetic advances in neurosurgery. Proc R Soc Med, 1970; 63: 821-825.[DOI]
[4] Ganslandt O, Merkel A, Schmitt H et al. The sitting position in neurosurgery: indications, complications and results. a single institution experience of 600 cases. Acta Neurochir, 2013, 155: 1887-1893.[DOI]
[5] Haji Mohd Amin MZ, Beng JTB, Young BTY et al. A case of cardiac arrest due to air embolism during scoliosis surgery. J Orthop Surg Res, 2019; 27: 2309499019840083.[DOI]
[6] Staartjes VE, Schillevoort SA, Blum PG et al. Cardiac Arrest During Spine Surgery in the Prone Position: Case Report and Review of the Literature. World Neurosurg,, 2018; 115: 460-467.[DOI]
[7] Miyakoshi N, Hongo M, Kasukawa Y et al. Intraoperative Visible Air Bubbling Recorded as a Sign of Massive Venous Air Embolism During Prone Position Surgery for Extensive Ossification of Spinal Ligaments: A Case Report with a Video Clip. World Neurosurg, 2019; 131: 38-42.[DOI]
[8] Cruz AS, Moisi M, Page J et al. Venous air embolus during prone cervical spine fusion: case report. J Neurosurg Spine, 2016; 25: 681-684.[DOI]
[9] Zhao SL, Zhang XY, Xiao Y et al. Gas Embolism After Hydrogen Peroxide Use During Spine Surgery: Case Report and Literature Review. World Neurosurg, 2020; 143: 228-231.[DOI]
[10] Zou P, Yang JS, Wang XF et al. Oxygen Embolism and Pneumocephalus After Hydrogen Peroxide Application During Minimally Invasive Transforaminal Lumbar Interbody Fusion Surgery: A Case Report and Literature Review. World Neurosurg, 2020; 138: 201-204.[DOI]
[11] Lang SA, Duncan PGM, Dupuis PRM. Fatal air embolism in an adolescent with Duchenne muscular dystrophy during Harrington instrumentation. Anesth Analg, 1989; 69: 132-134.[DOI]
[12] McCarthy RE, Lonstein JE, Mertz JD, Kuslich SD. Air embolism in spinal surgery. J Spinal Disord, 1990; 3: 1-5.[DOI]
[13] Albin MSM, Ritter RR, Pruett CE et al. Venous air embolism during lumbar laminectomy in the prone position: report of three cases. Anesth Analg, 1991;73: 346-349.[DOI]
[14] Horlocker TT, Wedel DJ, Cucchiara RF. Venous air embolism during spinal instrumentation and fusion in the prone position. Anesth Analg, 1992; 75: 152-153.[DOI]
[15] Sutherland RW, Winter RJ. Two cases of fatal air embolism in children undergoing scoliosis surgery. Acta Anaesthesiol Scand, 1997; 41: 1073-1076.[DOI]
[16] Pham Dang C, Pereon Y, Champin P et al. Paradoxical air embolism from patent foramen ovale in scoliosis surgery. Spine, 2002; 27: E291-E295.[DOI]
[17] Wills J, Schwend RM, Paterson A et al. Intraoperative visible bubbling of air may be the first sign of venous air embolism during posterior surgery for scoliosis. Spine, 2005; 30: E629-E635.[DOI]
[18] McDouall SF, Shlugman D. Fatal venous air embolism during lumbar surgery: the tip of an iceberg? Eur J Anaesthesiol, 2007; 24: 803-805.[DOI]
[19] Dumont TM, Stockwell DW, Horgan MA. Venous air embolism: an unusual complication of atlantoaxial arthrodesis: case report. Spine, 2010; 35: E1238-E1240.[DOI]
[20] Aurora S Cruz, Marc Moisi, Jeni Page et al. Venous air embolus during prone cervical spine fusion: case report. J Neurosurg Spine, 2016; 25: 681-684.[DOI]
[21] Lee-Archer PF, Chaseling B. Air embolism during posterior spinal fusion in a 10-year-old girl: a case report. A A Case Rep, 2017; 8: 307-309.[DOI]
[22] Goswami S, Brady JE, Jordan DA et al. Intraoperative cardiac arrests in adults undergoing noncardiac surgery: incidence, risk factors, and survival outcome. Anesthesiology, 2012; 117: 1018-1026.[DOI]
[23] Sprung J, Warner ME, Contreras MG et al. Predictors of survival following cardiac arrest in patients undergoing noncardiac surgery: a study of 518,294 patients at a tertiary referral center. Anesthesiology, 2003; 99: 259-269.[DOI]
[24] Quinn TD, Brovman EY, Aglio LS et al. Factors associated with an increased risk of perioperative cardiac arrest in emergent and elective craniotomy and spine surgery. Clin Neurol Neurosurg, 2017; 161: 6-13.[DOI]
[25] Girardi LN, Barie PS. Improved survival after intraoperative cardiac arrest in noncardiac surgical patients. Arch Surg, 1995; 130: 15-18.[DOI]
[26] Klein J, Juratli TA, Weise M et al. A Systematic Review of the Semi-Sitting Position in Neurosurgical Patients with Patent Foramen Ovale: How Frequent Is Paradoxical Embolism? World Neurosurg, 2018; 115: 196-200.[DOI]
[27] Chhabra A, Pathak P, Ray R. Fatal posterior fossa pneumocephalus due to hydrogen peroxide irrigation of lumbar wound. Brit J Neurosurg, 2000; 14: 549-551.[DOI]
[28] Kleffmann J, Ferbert A, Deinsberger W et al. Extensive ischemic brainstem lesions and pneumocephalus after application of hydrogen peroxide (H2O2) during lumbar spinal surgery. Spine J, 2015; 15: e5-e7.[DOI]
[29] De-Giorgio F, Arena V, Turturro F et al. 11 year-old girl undergoing scoliosis surgery. Brain Pathol, 2012; 22: 571-574.[DOI]
[30] Zhang J, Zhang C, Yan J. Massive cerebral gas embolism under discectomy due to hydrogen peroxide irrigation. Case Rep Neurol Med, 2015; 2015: 497340.[DOI]
[31] Bienert GP, Schjoerring JK, Jahn TP. Membrane transport of hydrogen peroxide. Biochim Biophys Acta, 2006; 1758: 994-1003.[DOI]
[32] Mut M, Yemisci M, Gursoy-Ozdemir Y et al. Hydrogen peroxide-induced stroke: elucidation of the mechanism in vivo. J Neurosurg, 2009; 110: 94-100.[DOI]
[33] Rodriguez RA, Sinclair B, Weatherdon D et al. Patent foramen ovale and brain micro-embolization during scoliosis surgery in adolescents. Spine, 2001; 26: 1719-1721.[DOI]
[35] Moe JH, Winter RB, Bradford DS et al. Scoliosis and other Spinal Deformities. Philadelphia, W. B. Saunders Company, 1978.
[36] Albin MS, Carroll RG, Tung AL. Venous air embolism in the sitting, lateral, supine and prone positions. Presented at the International Anesthesia Research Society 51st Congress, Hol lywood, FL, March 1977.
[37] Adoranto DC, Gildenberg MD, Ferrario CM et al. Pathophysiology of intravenous air embolism in dogs. Anesthesiology, 1978; 49: 120-127.[DOI]
[38] Albin MS, Carroll RG, Maroon JC. Clinical considerations concerning detection of venous air embolism. Neurosurgery, 1978; 3: 380-384.[DOI]
[39] Hybels RL. Venous air embolism in head and neck surgery. Larygoscope, 1980; 90: 946-954.[DOI]
[40] Michenfelder JD. Air embolism. In: Orkin FK, Cooperman LH (ed). Complications in anesthesiology. Philadelphia: Lippincott Company, 1983: 268-273.
[41] Holt EP, Webb WR, Cook WA et al. Air embolism: hemodynamics and therapy. An Thorac Surg, 1968; 2: 551-560.[DOI]
[42] Hartveit F, Lystad H, Minken A. The pathology of venous air embolism. Br J Exp Pathol, 1968; 49: 81-86.





 Copyright ©
Copyright ©